Messy moments: Generational conflict among colleagues
The generational divide can be a source of friction between coworkers.
Scenario
A nurse tells the managing MD that you did not order tests she thinks necessary for a patient.
He takes you, a junior MD, aside to say the usual practice is to order X and Z tests for those symptoms.
The millenial MD responds: “I see AB as the likely problem, so that’s the first and most important thing to rule out …”
The senior MD interrupts:“You’re relatively new here. We’ve been doing this for years...”
The millennial MD feels dismissed. The senior MD communicates that he doesn't care what you think. Just get with the program.
What would you like to happen?
You want colleagues’ respect for you and your experience… in actual daily interactions. You want to be involved and trusted in decision-making.
You want to know your care team talks with you -candidly and directly.
You want to be treated as someone who belongs and is valued. You’d like to understand exactly what happened here: differences in age, gender, ways of expressing yourselves, old-fashioned rank?
You want the complicated business of decision-making to be a better experience for everyone involved.
What you can do
On your own
- It’s understandable that you feel dissed and dismissed. Find a quiet space to pause. Breathe slowly for a moment.
- Label what you feel – frustration, anger, disappointment, threatened, not-good-enough…
- Then step away from the emotion. Accept it and put it to the side. It’s critical for you to move strong emotions - feeling victimized, attacked, insulted – aside because they strangle clear thinking. Ask yourself what you need now to retain your dignity and ability to practice.
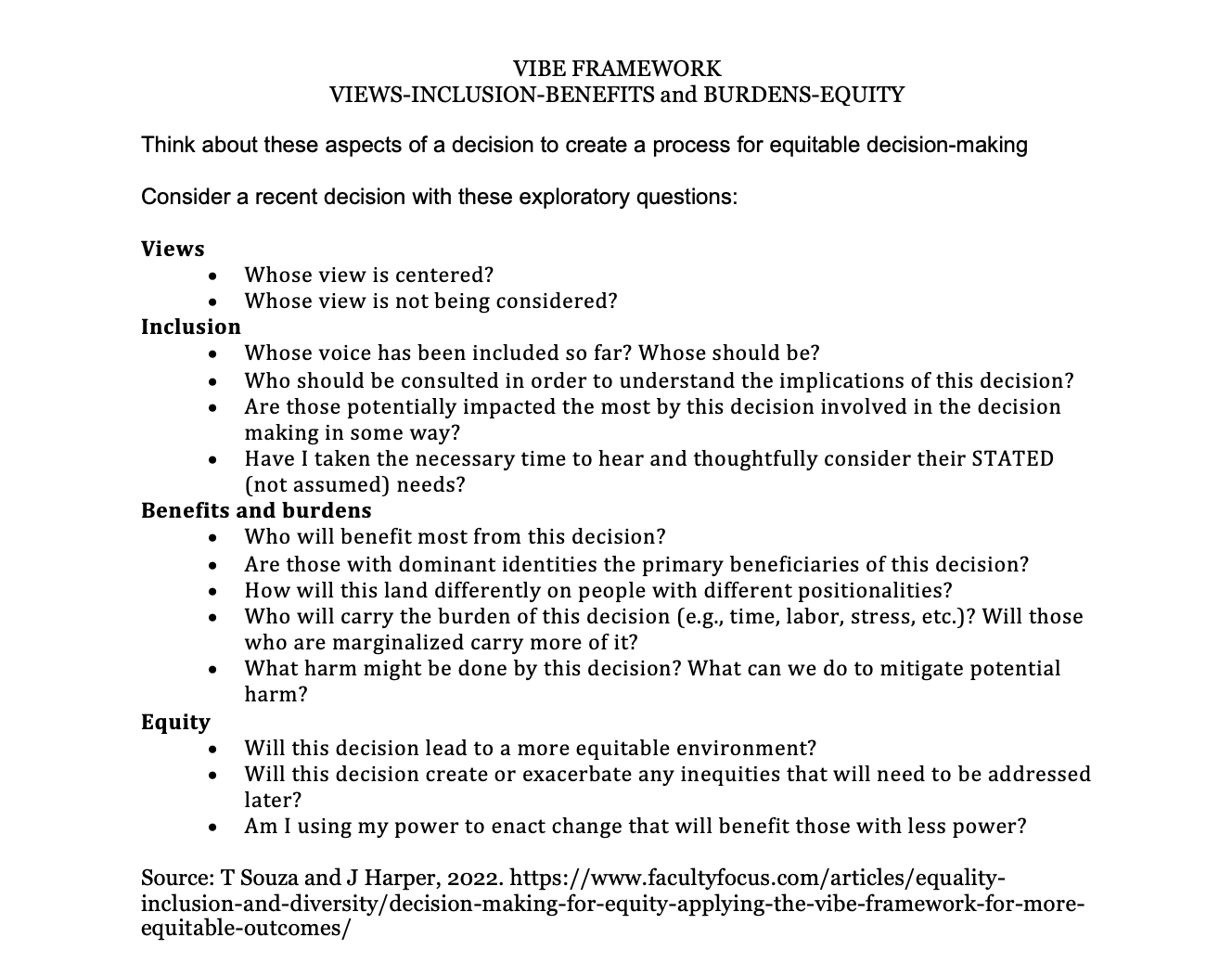
- Use the VIBE framework for more equitable participation in decisions [see worksheet below]
Talk with others
- Talk to others MDs in other practices colleagues to see what they’ve experienced and how they dealt with it.
- Talk to a senior colleague you trust inside or outside the practice. Ask what they recommend as a response to a pattern of pulling rank and silencing. This bullying pervades medicine. It’s long been a norm.
- However, organizations committed to inclusivity and care quality must support thought over silence and the voice of everyone relevant to a decision.
Talk with the Senior MD
- Ask the senior MD to suggest a time to talk.
- Plan the words you’ll use to tell him how you’d like to hear criticism, disagreement, new information. Words matter.
- Do what helps you feel calm, composed, and courageous.
- Focus on solutions.
- Create a frame: you both want a good diagnosis and decision.
- Then talk with him how you can together better assess complex situations and address a difficult diagnosis. And how to help each other.
- Clearly communicate that your relationship with him is important to you.
- Be specific about the challenge and open-ended in discussion of possible solutions.
- Tell him that you’d like to be asked what you think when you disagree. And you’d like to hear his thinking. “Tell me why you think that?” He may have no idea how to disagree respectfully.
- Offer a learning opportunity: Suggest that the practice meet to discuss recent confusing clinical cases. Invite others to present case problems -so it’s not just about you! You’ll create community learning and language for discussing complex, uncertain situations.
Benefits
- You improve the chances that senior clinicians will listen to you by trying to understand their perspective and highlight your mutual interests.
- Our assumptions, beliefs, previous experiences and fears determine how we interpret others’ behaviors. We often think they mean something very different from what they intend. Finding out what’s going on with them, then offering shared aims places you in their world.
- Explaining how you’d like to hear comments on your work tells senior people that you want to learn from them.
- The senior MD may not have had any intention of insulting or excluding you. It’s the way he’s done things in the past.
- If it continues to happen, bring someone else into the conversation.
- Your courage in speaking thoughtfully and respectfully make it easier to speak up next time.
- Bullying and exclusion behaviors are habitual and often tolerated by others as a norm.
- Your voice changes that for you and for others.
- Collegial discussions of confusing cases offers learning for everyone. It also reduces the threat from discussing decision-making. It shifts from two conflicting individuals to common workplace interactions. It builds trust and everyone learns about new factors important to decision-making.
- Clinicians able to talk with one another about opposing ideas prove critical to better and faster patient decisions.
- Success in improving equity requires not only high level commitment but also achieving voice and equity in decision-making at all levels down to the bedside.
- Collaborative decision-making based on clear norms, defined roles and shared purpose improve everyone’s adaptability and agency in complex, changing care.
This problem pervades the hierarchical and judgmental environment of medicine. Speaking up may have negative consequences.
Silence, though, undermines and isolates you.
“After the twelve-thousandth time, it starts to impede your ability to be successful. You start to go into scenarios about your self-worth….” - Dr. Sheryl Heron, a Black professor of emergency medicine, Emory University School of Medicine
Speaking clearly brings you into the room. You show that you too really want high quality patient care
Talking to others make the issue visible and brings you into the community. That in itself can fuel change.
Have you experienced senior staff pulling rank and silencing you? What did you do and how did that go? I’d really like to know. Email me and ask any questions you have for a future messy moment.