Technology Survey 2010: Uncle Sam's EHR Incentives
If you’re confused about the federal incentives to buy an EHR and what meaningful use means, you're not alone. We have the answers in our 2010 Technology Survey.
Want to avoid an expensive misstep when shopping for an EHR? Look for unbiased advice and go with your gut, says Deanna Attai. The Burbank, Calif., breast surgeon says she didn’t know that the EHR vendor she selected had paid for its glowing references. Worse, she didn’t follow her instincts. She has spent an additional $30,000 so far replacing that feature-rich system that never panned out.
Attai has a different system today but also more wisdom. “I should have listened more to my gut and not been distracted by the bells and whistles they promised but didn’t deliver,” she says.
With the government now offering cash incentives for implementing an EHR, many physicians who’d long held out have had their interest piqued, even as others remain skeptical, according to the 2010 Physicians Practice Technology Survey.
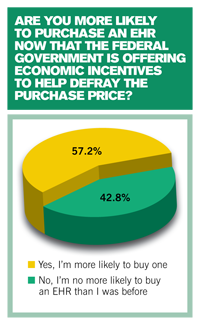
More than half (57 percent) of the 597 respondents to our survey told us that the Medicare and Medicaid-based incentive programs set to launch in 2011 make them more likely to buy an EHR. Getting cash from the federal government to defray the cost of an expensive purchase sounds appetizing. But like most lunches, this one really isn’t free; Uncle Sam isn’t offering to take you EHR shopping. Only after practices front the money to buy a “certified” system and follow the just-finalized rules for demonstrating that they are meaningfully using it can they seek federal stimulus dollars. And these facts have most physicians still puzzling over how the whole program will work.
We’ll help sort that out as we take a closer look at this year’s technology survey results.
The HITECH act
First, some recent history.
The EHR incentive program was created by the Health Information Technology for Economic and Clinical Health Act (HITECH Act), part of the federal stimulus package signed by President Obama in 2009. The legislation provides incentives to each physician (and certain other providers) who meet HITECH’s requirements. You can participate in the Medicare or the Medicaid incentive program, but not both. Switching between incentive programs after you start is allowed, but only once.
The legislation sets four objectives for physicians to get the stimulus money. You must:
• Use certified EHR technology in a
meaningful way;
• Utilize electronic prescribing;
• Use a system that electronically exchanges health information to improve the quality of care; and
• Submit information about clinical quality and other measures.
To meet that first bullet, the Centers for Medicare and Medicaid Services (CMS) sets 15 mandatory requirements for eligible providers (and 14 for hospitals) to meet in 2011 and 2012. Eligible providers and hospitals also must meet at least five additional measures of their choosing from a menu of 10 requirements. CMS plans to raise the bar by adding more criteria in subsequent years of the bonus program.
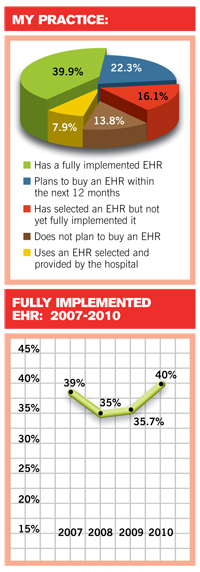
Incentives over time
About 40 percent of office-based physicians are already using fully integrated EHR systems, according to our survey. A 2009 survey conducted by the Centers for Disease Control and Prevention found similar numbers, although other estimates put the number of EHR adopters lower. One problem is that EHR adoption seems to have stalled: our first Technology Survey in 2005, for example, found the same 40 percent rate. The bonus payments to physicians and hospitals are seen as necessary to jumpstart EHR systems, which in turn is seen as crucial to moving Americans into a system of care that’s comprehensive and, eventually, cheaper.
Medicare offers physicians a bonus of up to $44,000 paid over a five-year period starting in 2011 (a separate program for hospitals begins Oct. 1, 2010). The payments are tied to 75 percent of your annual allowed Medicare Part B charges that year. If you start in 2011 or 2012, you can capture the maximum $18,000 bonus in your first year of participation by billing at least $24,000 in Medicare allowed charges. Participation in the bonus program ends in 2015, so waiting until 2013 to begin drops your cumulative take to $39,000 and to $24,000 if you start in 2014.
The Medicaid bonuses are geared to patient volume and there’s no penalty for not participating. At least 30 percent or more of your patient volume must be Medicaid beneficiaries (but only 20 percent for pediatricians) measured over any continuous 90-day period in the program’s first calendar year. Eligible professionals for Medicaid bonuses include nurse practitioners, certified nurse-midwives and some physician assistants such as those working in rural health clinics or provider shortage areas.

For both programs, CMS will make bonus payments to each eligible professional in your practice. In other words, a group of three internists could receive $132,000 in total if each successfully participates in the Medicare program. But can they get there in time?
To earn the bonuses, you’ll first need to meet the criteria set by CMS - from maintaining medication and allergy medication lists electronically for the majority of your patients (from all payers, not just Medicare and Medicaid) to providing patients with electronic copies of their health records upon request. Find the full criteria and other rules on the CMS Web site. Blumenthal, the ONC director, compiled a helpful, user-friendly chart for the New England Journal of Medicine that contains the full list of mandated and elective criteria.
The rule calls for attesting in writing to using your EHR to those capabilities for at least a 90-day period if you start during 2011 and for a full year if you start in 2012 or later. Plus you’ll
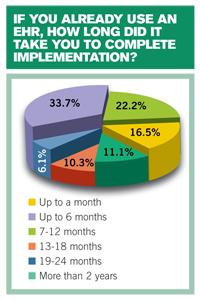
need to submit quality data electronically. Seems reasonable. Or is it? If you aren’t close to purchasing your EHR now, consider this: 40 percent of our survey’s respondents said they spent four months to a full year shopping for the right EHR - and one in four spent more than a year. And that’s just getting to the purchase decision. More than half (56 percent) of you said it took six months to a year to complete implementation, while one in 10 needed up to 18 months.
Do the math from today and it could be a challenge to hit all of the required CMS targets for meaningful use by the end of 2011.
“The problem with setting these across-the-board thresholds is that the government is requiring the eligible provider to rely on the cooperation of a third party,” says Robert Tennant, senior policy adviser for the Medical Group Management Association. For example, the proposed rules would have required that 75 percent of physicians’ prescriptions be generated and transmitted electronically. Tennant complained that such a high hurdle “could be a problem when practices deal with small pharmacies that haven’t set up e-prescribing, or with patients who want paper scripts because they don’t have a “regular pharmacy.” Other physicians’ advocates voiced similar complaints. The final rule, released in mid-July, lowers the e-prescribing threshold to 40 percent.
Many observers have recalled the CMS’ pay-for-performance program, called the Physician Quality Reporting Initiative (PQRI), as an example of how a well-intentioned program can ensnare physicians in unfair rules that prevent doctors who participated in good faith from receiving the promised bonus in a timely fashion. The PQRI program promised bonus money to doctors who reported certain quality data correctly, but CMS did not deliver first-year results to many participating physicians until well into the next reporting year, too late for them to adjust their reporting and qualify for the incentives. Many failed to receive the promised bonuses while payments to others were delayed.
“Yes, the financial incentives are significant,” says Tennant, “but there are a lot of hoops to jump through and, remember, this is spread out across five years with the requirements steadily increasing.”
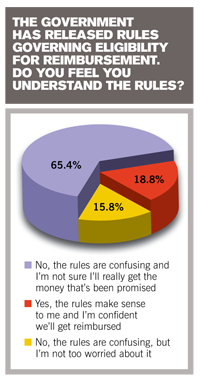
Indeed, two-thirds of you told us in the survey that the proposed EHR reporting criteria are confusing and you don’t expect to get the money.
Instead of a big haul, consider funds from the government’s reimbursement incentive a sweetener for making a transition you will probably have to do sooner or later, Tennant says.
“If the bonus is the only reason you are moving to an EHR, you’re probably going to fail. Think about the extra value of EHR in transforming your practice, both on the clinical side and on the administrative side to reduce costs and increase revenue.”
Existing systems can qualify
To qualify for the Medicare and Medicaid bonuses, your EHR system must to be certified. In June, David Blumenthal, MD, director of the Office of the National Coordinator for Health Information Technology (ONC), which is handling the certification process, announced its plan for one or more organizations to certify EHRs, or individual EHR modules, such as e-prescribing software, under the HITECH Act.
Certification is a critical element both to new EHR purchasers and current system owners. While the legislation permits you to obtain stimulus funds for any certified system you use, even if you purchased, implemented, and paid for it years ago, your software must be certified under the new meaningful use criteria. ONC will post on its Web site all certified software products that qualify their users for the incentives.
Vendors are moving fast: In order to meet the Jan. 1, 2011, program starting date, they must reconfigure their systems to conform with the meaningful use criteria, achieve certification, and install or upgrade the systems at customers’ offices by the end of 2010.
Even those who purchased advanced systems from solid companies are finding out that, sometimes, well, stuff happens. Just ask Boca Raton, Fla., internist Steven Reznick. Five years ago, Reznick and his practice partner picked the most advanced EHR they could afford from the most solid company they could locate. They forked over some $60,000 to buy software, hardware, and pay for training and maintenance packages. A few years later, surprise: the company was purchased by a larger firm that will discontinue support for Reznick’s software at the end of 2011. The cost of migrating to the new system will be about $10,000.
“I’m 60 years old. I have a small practice and hope to practice another 10 years, but if I didn’t already have an electronic health record, would I want to invest a large amount of money … today?” he said. “Probably not.”
Return on investment?
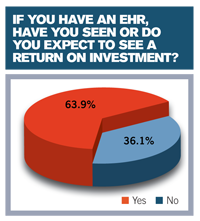
Nearly two-thirds of you (64 percent) said you expect a return on investme
nt from your EHR purchase, or already have received one. Reznick and Attai are confident they are seeing the benefits in their practices, even with the vendor problems they’ve experienced.
Measuring the return won’t be easy, says Paul Solverson, management consultant partner with Affiliated Computer Services, Inc., a Xerox Company. “At the end of the day, physicians are going to have spent at least as much as they are going to get from these reimbursement incentives,” Solverson says. “The ones who get the most out of an EHR will be the ones who embrace this as a positive change, not something they have to do to avoid a penalty.”
Solverson says that when measuring the ROI, the biggest wild card is figuring the costs and benefits of changing work flow necessary for a successful implementation.
“It’s difficult to pinpoint a single, best-practice, work flow change that happens with EHR but it’s safe to say that the more you can implement the technology for real-time use, the better the outcome,” he explains.
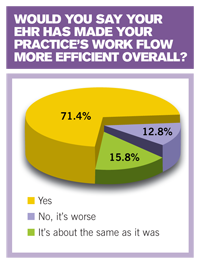
A whopping 71 percent of our survey respondents said they expected work flow improvements as a result of implementing an EHR.
Gina Tucker, administrator of Hampshire OB-GYN in Northampton, Mass., says she has proof of those improvements. As an early adopter of EHR back in 2004, the practice of five physicians, five NPs, and a nurse-midwife now achieves every aspect of the clinical and administrative activity needed to complete a patient visit - even a coding review and CPT-to-ICD matching - by the time the patient leaves the office.
That level of integration wasn’t entirely due to the Hampshire EHR’s smooth interface with a practice management system, though that helps. What it took was a willingness to re-examine protocols for every activity, from documenting phone calls to sending laboratory orders.
“It is a big upheaval in one sense but we looked at it as a way to improve the practice and improve patient safety,” Tucker says. “You need people who are willing to accept that the way they’ve done things is going to change.”
Solverson recommends getting an office administrator and a key clinician, such as a nursing supervisor, to work with the physicians to analyze how the EHR will change work flow. Practice leaders must also take the lead in designing an implementation plan that could include, sometimes, breaking down walls between office functions that traditionally stand separate, such as the billing office and the front desk.
So what’s a physician to do? Steven Lazarus, president and founder of the Boundary Information Group of consultants in Denver, suggests accelerating your education about EHR.
“Don’t waste time getting started if you know it is something you want to do,” Lazarus says. “You will run out of time to qualify for bonuses and finding outside help will be harder if everyone else is asking at the same time.”
Lazarus suggests:
• Read up. Books, magazines, white papers, and reports from government, nonprofit organizations, and private sector companies are out there to help novices and experts alike.
• Get educated. The HITECH Act funds 60 federally designated Healthcare Information Technology Regional Extension Centers (RECs) across the nation. These centers will provide no-cost and low-cost seminars, summits, online education, and technical advice to help physicians quickly implement and become adept users of EHR. See a list of all 60 centers online.
• Examine vendors. Lazarus suggests looking for vendors with good track records on customer surveys and adequate capacity to handle a big influx of new customers.
• Look for help soon. Hiring qualified technical help, whether it’s a new staff member or a consultant, will be harder if thousands of other medical practices are doing the same thing at the same time as you.
• Give incentives and seek penalties. With good help in short supply, and a likely sellers’ market for EHR, Lazarus suggests writing financial incentives into contracts with vendors: promise them a small bonus for a successful implementation, but also seek a similar-sized penalty if they let you down.
• Be aware and beware. Get a knowledgeable technology attorney to review any agreements with a vendor. Your general legal counsel may not have the expertise needed to review software licensing clauses, limitations, and other unique aspects of an EHR agreement, Lazarus says.
Worried about the Medicare or Medicaid reimbursement penalty you’ll suffer if you don’t hit the government’s EHR targets? Sit down and figure out what a maximum 3 percent penalty on your Medicare income comes out to in dollars. Then run the numbers at 5 percent, which is what HITECH allows the government to remove from Medicare reimbursement starting in 2019. Maybe there’s no need to panic.
In the long run, practices still using old-fashioned paper will become the analog outsider and experience a significant competitive disadvantage in the world of digital medical communications. So it’s time to get moving on your EHR transition, if you haven’t already.
You should not rush. But you should hurry.
View all survey results here.
Bob Redling is a freelance writer based in Tacoma, Wash. He has been practice management editor for Physicians Practice, Web content editor and senior writer for the Medical Group Management Association, and a speechwriter for the American Academy of Family Physicians. He can be reached via physicianspractice@cmpmedica.com
In Summary
More than half of respondents to the 2010 Physicians Practice Technology Survey told us that the federal government’s Medicare and Medicaid EHR incentives have them shopping for a system. If that’s you, or you already have an EHR, here’s what’s needed to get the promised reimbursement bonuses:
• Use an EHR that meets standards and certification criteria set by the Office of the National Coordinator for Health Information Technology (ONC).
• Meet CMS’s 15 mandatory requirements (14 for hospitals) for meaningful use during 2011 and 2012 (and 2010 if starting early).
• Select at least five additional measures from the 10 provided by CMS.
• Prepare for criteria to expand in 2013 and subsequent years of the program.
• Stick with the program for the full five years (Medicare) or six years (Medicaid) to earn the full reimbursement bonuses.
Start now looking into systems, vendors, and sources of expert help because thousands of other physicians may also be EHR shopping.
Read More About It
Need more information about EHR adoption and the rules of the government’s EHR stimulus program? Check out these additional sources:
• A list of the 15 mandated meaningful use criteria, and the “menu” of 10 criteria from which physicians must select five:
• Technical fact sheets and FAQs about CMS’s incentive programs
• A technical fact sheet on ONC’s standards and certification criteria final rule
• A fact sheet about the HITECH Regional Extension Program
• A list of Health Care Technology Regional Extension Centers (RECs)
• CDC Survey on EHR adoption
View all survey results here.
This article originally appeared in the September 2010 issue of Physicians Practice.
HIPAA highlights: 2 disturbing class actions, OCR risk analysis enforcement
April 24th 2025Two class-action lawsuits targeting the University of Maryland Medical Center and the University of Kansas Health System for years-long cyberstalking and unauthorized access to protected health information spotlight massive HIPAA risk-analysis failures and underscore the urgent need for stronger health care cybersecurity safeguards.