Tackling the biggest problems with your billing
Adding appropriate technology to your practice can have profound effects on the well-being of your operations, allowing your workforce to focus on what they do best while you concentrate on patient care.
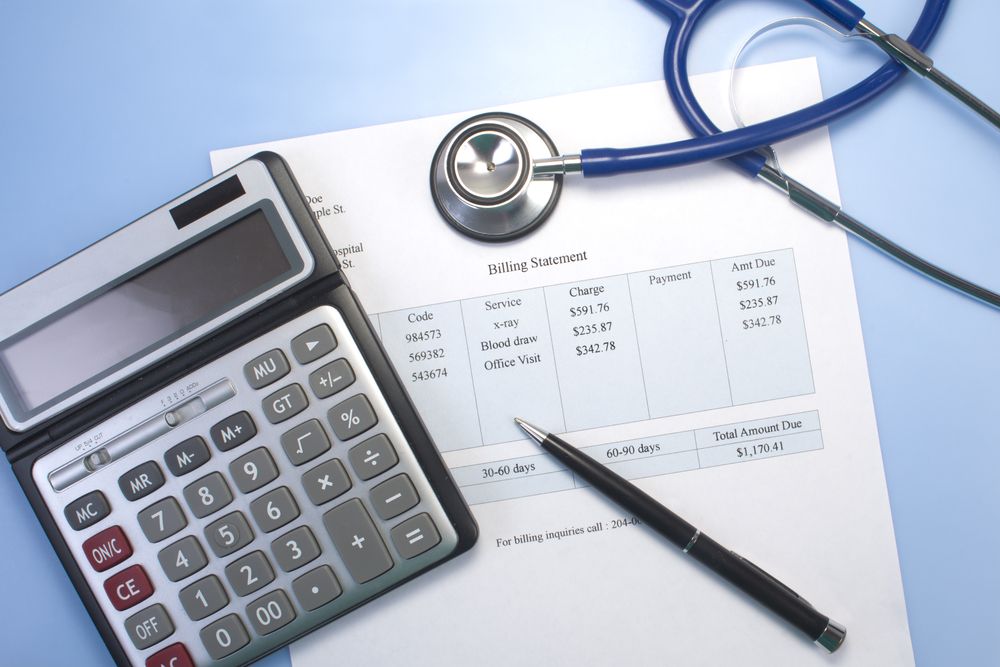
Sherry Yates Young / Shutterstock
When it comes to the financial health of your practice, nothing has a greater impact than the people behind your billing. Whether in-house or outsourced, you need a team you can trust - and one with the experience to do the job right.
A recent Quest Diagnostics survey of more than 300 private practice owners, co-owners and partners provides insight into the greatest pain points related to physician billing. A closer look reveals opportunities for practices to potentially improve the financial health of their businesses while reducing the time spent handling claims, coding and educating staff about the evolving reimbursement landscape.
The varying requirements from payers pose a continuous challenge to physicians who find themselves facing tighter time constraints and declining reimbursements. It can be difficult to stay current with payer contracts, payment schedules and changing rates for commonly used codes.
Just knowing the correct nomenclature is yet another challenge, and the International Classification of Diseases (ICD) is a prime example. The move from ICD-9 to ICD-10 in fiscal year 2017 brought us from approximately 13,000 codes to more than 87,000. Navigating that many procedures and entries has proven daunting for many providers and their staff.
Many offices have a receptionist, an office manager and a medical assistant. When it comes to keeping up with billing and reworking claims, however, physicians reported in the Quest survey that it’s difficult for this limited staff to maintain the focus necessary, as they simply have too many other demands in a busy office. Frequently, the available employees lack the necessary experience and expertise to manage accurate and efficient billing procedures.
Adding appropriate technology to your practice can have profound effects on the well-being of your operations, allowing your workforce to focus on what they do best while you concentrate on patient care.
Getting a hold of the process
Increasingly, clinicians are adding practice management (PM) software that can reduce administrative tasks, such as scheduling and appointment reminders. Others are outsourcing the billing process altogether. Many practices are exploring revenue cycle management (RCM) providers, seeing it as an ounce of prevention for common revenue problems reported by those struggling with in-house billing.
Practices that perform in-house billing can benefit from properly integrated PM software to maintain patient communications while manually handling many billing procedures. It is imperative that someone responds to rejected and denied claims in a timely manner and that person also stay on top of regulatory changes.
A comprehensive RCM solution removes much of that burden from your team and may make for more timely reimbursements. These tasks would be handled by a service for a percentage of collections or for a subscription fee.
An RCM provider can also handle patient payment collection and claim reviews from insurance companies - common tasks within the revenue cycle - that can be a challenge for many practices. In fact, an enhanced RCM can help avoid issues before they occur. When these functions are properly combined with an electronic health record (EHR) or PM software, physicians can be alerted to potential issues, with the system flagging possible coding errors while still in the exam room.
12 RCM software must-haves
Should you decide to outsource your billing, consider an RCM that offers these key features:
- Management of denials, rejections and appeals
- Posting and monitoring of payments
- Printing, mailing and emailing of patient statements
- Convenient methods of accepting patient payments such as credit cards, online, or customized payment plans
- Administration of unpaid balances
- Timely processing of insurance payments
- Automated updating of fee schedules and contracts
- Detailed reporting functionality
- Dedicated customer service with regular consultations
- Thorough training and support
- Compliance with HIPAA, OIG and ICD-10 regulations
- Integrated EHR and PM software
By tackling the biggest problems head on, you can proactively engage with the fiscal fitness of your practice in a way that shows real results, all while working to increase your efficiency.
About the survey:
The Quest Diagnostics survey was conducted in July 2019 and had 325 respondents, of whom:
55% owner/co-owner/partner of private practice
21% employed by hospital or institution
29% group practice
3% accountable care organization
8% patient-centered medical home.
Tom Romeo is the general manager of healthcare IT and Quanum solutions at Quest Diagnostics.
Is your practice ready for the Trump tariffs?
April 7th 2025Tariffs are set to drive up costs across industries — including health care — impacting everything from medical supplies to retirement accounts. Take a look at the ripple effects on medical practices and some proactive strategies for physicians to stay one step ahead.