Suggestions for protecting your medical practice from litigation
Safeguard your medical practice from litigation by adopting proactive strategies.
© yavdat - stock.adobe.com

Litigation is an ever-present concern for medical practitioners. In 2022, 1.8 percent of all physicians were sued in the previous year. 31% of physicians have been sued at some point in their careers.1 On average, physicians spend nearly 11 percent of their 40-year careers with an open, unresolved malpractice claim.2 While providing medical care is a noble profession, it comes with inherent risks, including the potential of being involved in an emotionally painful and expensive lawsuit. Safeguard your medical practice from litigation by adopting proactive strategies that mitigate risks, promote patient safety, and ensure compliance with the law.
Here are a few strategies that may help protect you from litigation:
1. Informed consent
Before any treatment, procedure, or surgery, ensure that your patients fully understand the risks, benefits, and alternatives, even if the alternative is not to take your advice and do nothing. The informed consent should be written in non-medical jargon, and any medical terms should be defined. It is imperative to take time to address their questions and concerns. Document the informed consent process in the patient's medical record. Document the conversation in your records if there is any discussion about the consent.
2. Effective Communication
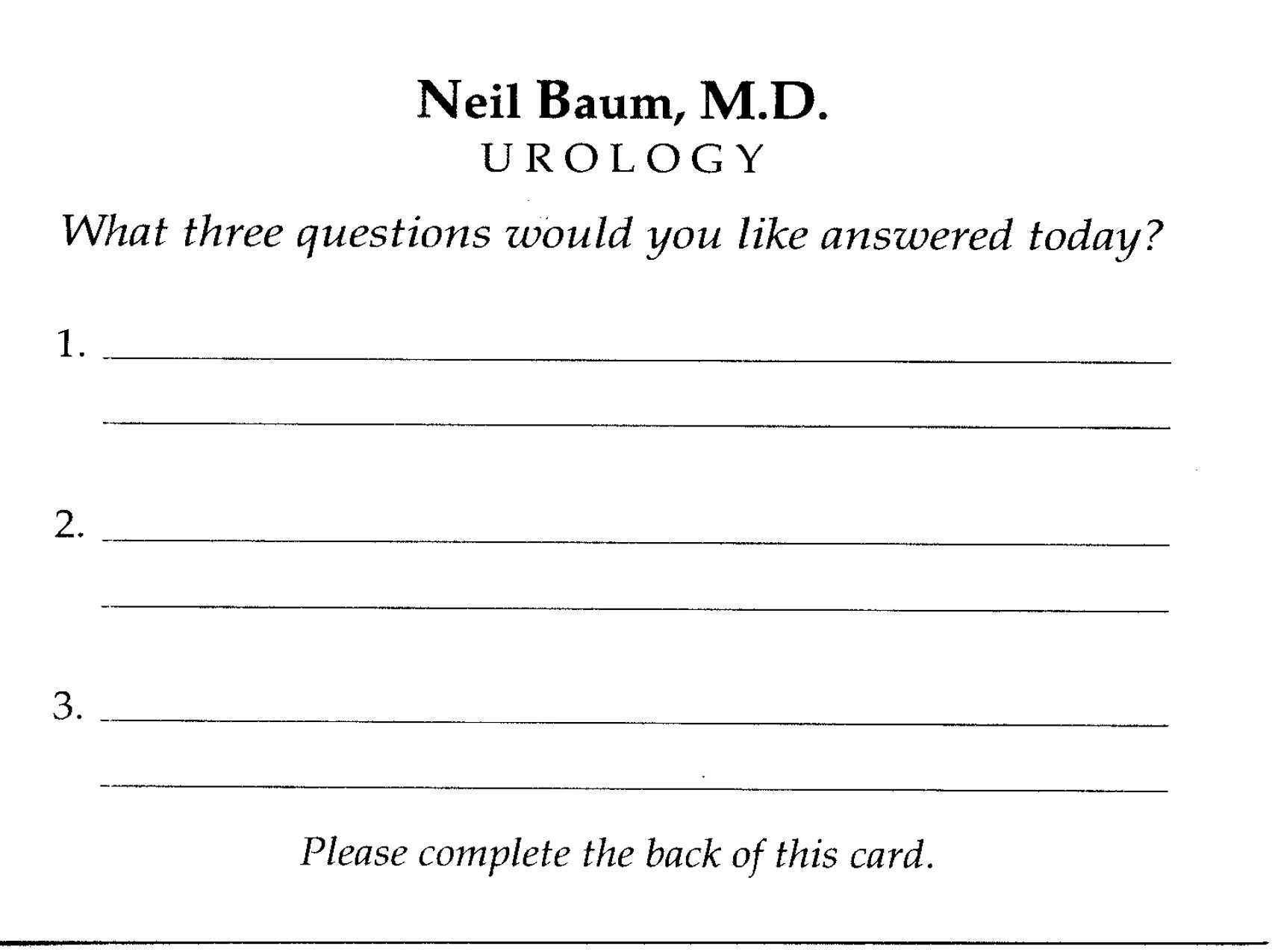
Effective communication is imperative for reducing the risk of litigation. Ensure you communicate clearly with your patients, addressing their concerns and explaining treatment options. Encourage open dialogue and actively listen to their questions and feedback. Misunderstandings or a lack of communication can lead to dissatisfaction and, ultimately, lawsuits. One suggestion for enhancing communication is ensuring you have answered all questions during the encounter. I have provided patients with a 3x5 card and encouraged them to write down any questions they want answered. Not only was I able to be sure that their questions were answered, but this card significantly decreased patients calling back to the office with questions that they should have remembered to ask when they were in the office.
3. Risk management
A risk management program identifies potential risks, analyzes their impact, and takes measures to prevent them. Regularly assess your practice's policies, procedures, and protocols. Identify areas where improvements can be made to reduce the likelihood of errors or adverse events. For example, I had to add an addendum to the policy manual regarding zero tolerance for sexual harassment.
4. Continuing education
You must stay current with the latest developments in your field. Participate in continuing medical education (CME) activities, attend conferences, and engage in peer discussions. This improves the quality of care you provide and demonstrates a commitment to ongoing learning, which can be a strong defense in litigation.
5. Patient safety
Prioritize patient safety in your practice. Establish a culture emphasizing safety, and regularly assess your systems and procedures. Encourage your staff to report incidents, near-misses, or unsafe conditions. Demonstrating a strong commitment to patient safety can mitigate the risk of adverse events and subsequent lawsuits.
6. Employee training
Ensure that your staff receives adequate training in their respective roles and responsibilities. Educate them on patient confidentiality, obtaining informed consent, and safety protocols. Well-trained staff can help prevent errors and misunderstandings that might lead to litigation.
7. Address patient complaints proactively
When a patient expresses dissatisfaction or files a complaint, do not ignore it. Address it promptly and professionally. Listen to the patient's concerns, investigate the issue, and respond respectfully and empathetically. Open lines of communication can often resolve disputes before they escalate into legal action. This is especially important for those experiencing an adverse event or a complication. Giving the patient your undivided attention when managing one of these situations will often alleviate the patient's angst and avoid a lawsuit.
8. Ethical practice
Ensure that you adhere to professional standards and ethically conduct yourself. Avoid any situation that might lead to conflicts of interest or compromise patient care. Upholding a high standard of ethics not only protects your practice but also builds trust and credibility with your patients.
9. Collaborate with legal professionals
Consider building relationships with legal professionals who specialize in healthcare law. These individuals can provide valuable guidance on legal matters, risk management, and compliance. Having legal counsel readily available can be an essential resource in the event of legal challenges.
10. Document and learn from adverse events
Adverse events will occur in any medical practice. Having a system in place for documenting and learning from these events is crucial. Analyze the cause, assess whether there were any system failures, and make necessary improvements. This proactive approach demonstrates your commitment to patient safety and can mitigate legal liability.
On one occasion, I treated a patient for prostatitis and prescribed ciprofloxacin. I received a call to see the patient in the intensive care unit. He had pulmonary insufficiency secondary to a drug-drug interaction between ciprofloxacin and theophylline. I then implemented a program that checks for allergies and drug-drug interactions for all medications I prescribed.
11. Professional boundaries
Maintaining professional boundaries is vital in healthcare. Patients should not feel uncomfortable or violated during their interactions with healthcare providers. Educate yourself and your staff about the importance of maintaining appropriate boundaries. Be cautious about personal relationships with patients, as this can create ethical and legal dilemmas.
12. Documentation
Accurate medical records are the best protection against a lawsuit. If a lawsuit arises, having well-maintained records can significantly affect your defense. Of course, keep the medical records the same when you are served with a lawsuit.
13. Malpractice insurance
Medical malpractice insurance serves as a safety net to protect you in the event of a lawsuit. Ensure you have the appropriate coverage for your specialty and practice size. Reviewing your policy regularly, once a year, is vital to guarantee that it adequately covers your needs.
Bottom line
Protecting your medical practice from litigation is a multifaceted endeavor that combines legal awareness, risk management, ethical conduct, and a commitment to patient safety. By implementing the strategies outlined in this blog, you can reduce the likelihood of legal challenges and ensure that your practice provides the highest standard of care while maintaining the trust and confidence of your patients. Legal challenges are never completely avoidable, but a proactive approach can go a long way in protecting your practice and your professional reputation. Remember that healthcare is a dynamic field, and it's essential to continuously adapt and evolve to meet the changing demands and expectations of patients and the legal landscape.
Neil Baum, MD, a Professor of Clinical Urology at Tulane University in New Orleans, LA. Dr. Baum is the author of several books, including the best-selling book, Marketing Your Medical Practice-Ethically, Effectively, and Economically, which has sold over 225,000 copies and has been translated into Spanish.
- Seabury, S. A., Chandra, A., Lakdawalla, D. N., & Jena, A. B. (2013).
- Health Affairs, 32(1), 111-119.
Is your practice ready for the Trump tariffs?
April 7th 2025Tariffs are set to drive up costs across industries — including health care — impacting everything from medical supplies to retirement accounts. Take a look at the ripple effects on medical practices and some proactive strategies for physicians to stay one step ahead.