Robust billing software can maximize reimbursements, keep practices honest
CMS has been playing hardball regarding claims, which should keep everyone honest while saving the federal government money.

Say what you want about the Centers for Medicaid & Medicare Services (CMS), but the federal government has gotten really good at ferreting out waste, fraud, and abuse in claims.
In September, the U.S. Department of Justice announced its largest-ever healthcare fraud and opioid enforcement action in history, which resulted in charges against 345 defendants and alleged fraud losses topping $6 billion. Those charged included more than 100 physicians, nurses or other licensed medical personnel, so there likely were many billers and coders among those indicted. Seventy-five percent of the claims were for telehealth visits, with $845 million related to substance abuse treatment centers and more than $806 million related to various other healthcare fraud and illegal opioid distribution.
The CMS Center for Program Integrity also announced the revocation of Medicare billing privileges for 256 medical professionals for alleged telemedicine fraud cases. That represents a record-breaking number of actions related to telehealth, the use of which skyrocketed during the global pandemic.
There’s no doubt about it: CMS has been playing hardball regarding claims, which should keep everyone honest while saving the federal government money.
Billers and coders play critical roles in patient care, making sure that claims are correct and properly submitted so the practice, ambulatory care center, rehab center, hospital, or other provider can be properly reimbursed. In order to do their jobs properly, billers and coders need the right software tools to check claims before they are submitted to payers to maximize reimbursement, to reduce the incidence of refiled claims and to protect both themselves and their employers from fraud charges.
Better claims processing = higher payments
Despite technological advances, the claims denial rate remains stubbornly high in healthcare, averaging between 5%-10%. That might not sound like much, but consider a 10% denial rate multiplied by the number of patients seen by a practice each day. The result is thousands in potential claim losses per week.
Even if every claim is successfully reworked and resubmitted, that effort represents a significant outlay in time and personnel. The cost to resubmit a claim has been pegged at between $25-$45, and many medical practices just write that off—leaving significant money on the table.
And just because a claim is accepted, that’s no indicator it’s coded correctly or that it accurately represents the breadth and depth of a medical encounter. As many as seven-in-10 claims that providers submit contain errors that can impact payment. The error could be simple—a mismatched name—or more complicated, like improper patient types or missing/incorrect patient identifiers.
Claims software can prevent many of these errors by comparing claims against a huge database of various payers, procedures, adjustments, and other data to help billers and coders get it right the first time. Be sure to ask potential vendors how often the database is refreshed. Payers can adjust reimbursement rates daily, so you want to access the correct codes for a particular day of service.
Even before the COVID-19 pandemic gripped the nation, CMS declared a public health emergency in late January, a declaration that has been renewed multiple times. As a result, countless claim codes have been reclassified or reworked to reflect current circumstances and how patients access care. For example, the methods and reimbursements for telehealth visits were greatly expanded as remote medicine skyrocketed in early spring.
Medical providers who don’t keep up on the billing front are losing out.
Going astray can be costly
Billing software is also important to protect providers from fraudulent billing practices. Interestingly, the False Claims Act dates to the U.S. Civil War and was originally designed to prevent fraud in the delivery of supplies to Union troops.
As it relates to healthcare, the False Claims Act covers a variety of potential offenses, including upcoding, falsifying treatment plans or medical records to justify payment, misrepresenting patients or services, or incorrectly coding the location of services. Fines can be up to three times the disputed amount, plus as much as $22,000 per claim and possible criminal prosecution.
Even without malicious intent, miscoding claims is no laughing matter. A study published in 2019 shows a strong correlation between fraudulent claims and substandard patient care. The study found that patients treated by a provider later excluded from the Medicare program for fraud and abuse were between 14%-17% more likely to die than similar patients treated by other providers. Those who committed fraud or abuse against Medicare were linked to about 6,700 premature deaths in 2013 alone.
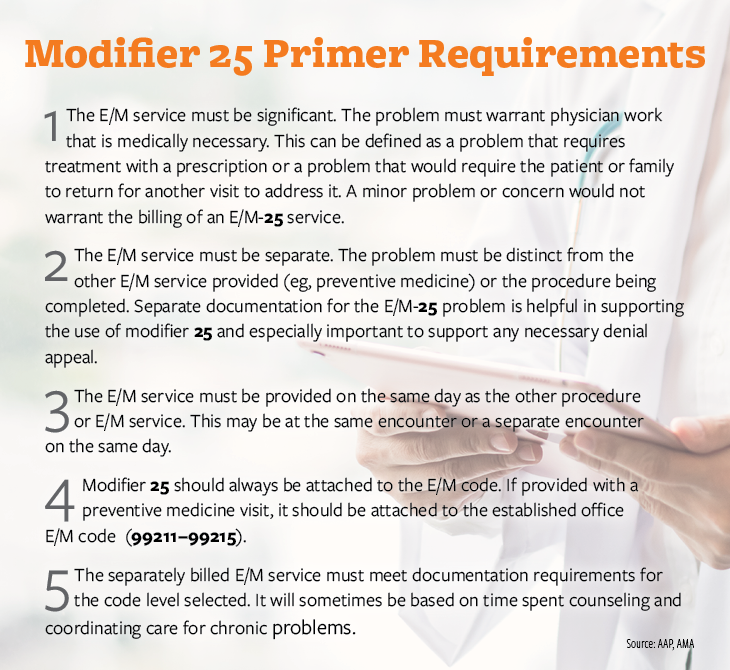
Other coding issues that can cause potential issues include the use of Modifier 25, which can be used to report an evaluation and management (E/M) service on the same day the physician provided another service for the patient, and Modifier 59, used for a distinct procedural service.
Billers and coders want to do their best to serve their employers and maximize reimbursements, so they need robust and frequently updated billing software. Such software can also help keep staff on the right side of the law.
About the Author
Andria Jacobs is the chief operating officer for PCG Software and has more than 25 years’ experience in the healthcare industry, encompassing both administrative and clinical arenas. Prior to joining PCG, Ms. Jacobs was the administrative director, medical management for VertiHealth Administrators. Previously, she was an independent consultant in ambulatory care and practice management, where her clients have included hospitals, physician groups, and the University of California, Los Angeles.
Is your practice ready for the Trump tariffs?
April 7th 2025Tariffs are set to drive up costs across industries — including health care — impacting everything from medical supplies to retirement accounts. Take a look at the ripple effects on medical practices and some proactive strategies for physicians to stay one step ahead.
Asset Protection and Financial Planning
December 6th 2021Asset protection attorney and regular Physicians Practice contributor Ike Devji and Anthony Williams, an investment advisor representative and the founder and president of Mosaic Financial Associates, discuss the impact of COVID-19 on high-earner assets and financial planning, impending tax changes, common asset protection and wealth preservation mistakes high earners make, and more.