MGMA 2020: Leading your practice through change
Change is a constant in healthcare, ensure your providers and staff are comfortable and confident as you move forward.

Change is almost synonymous with the healthcare industry. From new treatments to tech innovations, the consumerization of healthcare, continuing mergers/acquisitions, and disruptors like Amazon and telehealth, change is at the center of learning about and providing medical care. When it comes to implementing changes in your practice, there are a few key leadership responsibilities that will help you seamlessly integrate these initiates while guiding your staff to success.
At MGMA's virtual Medical Practice Excellence conference, Katie Lawrence, MHA, CMPE, director ambulatory optimization at Prisma Health, presented the session "Leading Organizations Through Change" and outlined the responsibilities of leaders in times of change and how you can anticipate various responses from your staff.
The first step in implementing change at your practice, Lawrence says, is self-reflection. There are three questions that you should be asking yourself before you propose changes to your team:
- What am I feeling about this change?
- Why am I feeling this way?
- Is what I am feeling helpful?
"Before your team sees you presenting a change, you need to know yourself how you're feeling about that change," says Lawrence. "And perhaps why are you feeling that way? Are you frustrated? Are you angry? Are you overwhelmed? Are you excited? Why are you excited? Why should they be excited?"
Lawrence says that most of us see and experience change in a four-stage curve. These are, respectively: denial, resistance, exploration, and commitment.
©2020 MGMA
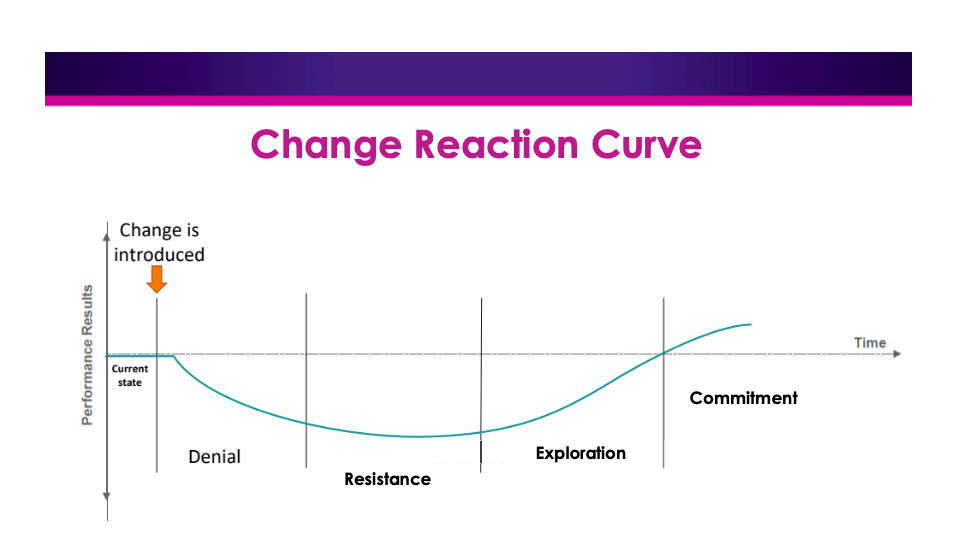
The transition from each stage is not necessarily as straightforward or as represented above.
"Each change is going to feel a little different, and each of those stages have different emotions that are attached and associated with it," Lawrence says.
A Leader's Responsibility
As previously stated, the primary responsibility of a leader introducing change to their team is to identify where he or she stands with that change.
"If you don't know where you are, it's really hard for you to be able to identify with someone else who may be in a different position or different place on that emotional curve," Lawrence says.
Once you have identified your own relationship with the proposed change and your place on the Change Reaction Curve, Lawrence says your next areas of concern as a leader will be to establish an atmosphere of psychological safety with your team and engage them in regular, effective communication.
Psychological Safety
All leaders, especially those in healthcare, should be aiming to establish a sense of psychological safety among their team, Lawrence says.
Members on your team, whether they be other healthcare providers or your staff, need to have confidence that they will not be embarrassed, rejected, or punished for speaking up or asking questions.
Some team members will have really good ideas, while others may have ideas that cannot be put into place; regardless, Lawrence says that no one's idea should be crushed nor disrespected.
To begin establishing a culture of psychological safety at your practice, Lawrence says that you can begin by welcoming feedback from your team. It's important to emphasize the invitation aspect because, she says, if you have never invited feedback before, your team will likely be hesitant to give it. Furthermore, they may be fearful of your reaction should their feedback be negative. Welcome the negative as well as the positive.
Rounding—a one-on-one meeting or session with your team—is another option where you foster this conversation. Unlike an open-door policy, the benefit here is that Rounding eliminates potential abuse of an open-door policy. Rounding also ensures that individuals that do not regularly take initiative to speak up have a chance to have their voice and thoughts heard.
Lawrence says that if you implement these tactics into your practice on a day-to-day basis, you will establish great trust among your team and staff.
Communication
While you start to engage in these regular communications with your team, Lawrence says you should keep in mind "Communication CPR".
- Candor — You should be honest without oversharing; embrace the positive and the negative; normalize discomfort; and consistently answer the 'Big 3': Why are we going through this change? What can I expect? What's in it for me?
- Recognize Positive Intent — Everything makes sense to the person saying or doing it, Lawrence says; however, this may not be readily clear to everyone else. Make a list of all of the pros and cons of a change, and then take a moment to stand in each provider's or staff's shoes to anticipate how they might react to the change.
- Maintain Respect — Make sure that the team member, physician, or stakeholder never looses dignity in your communications. Lawrence says that it is important to demonstrate intellectual humility.
Some predictable reactions to change that lead to failed change efforts include: a lack of understanding; a lack of sense of ownership; and a lack of capacity for change.
As a change leader, Lawrence says you should always:
- Create awareness of the change
- Encourage adoption
- Manage and coach for change
- reinforce the change
Lawrence also provides some response strategies to providers and staff on various points in the Change Reaction Curve.
For those in the Denial stage, create awareness of change by communicating, offering FAQs, and providing a path forward with milestones.
For providers or staff in the Resistance stage, encourage adoption by providing resources, de-prioritizing lesser important work, and asking for input
If a provider or staff member is in the Exploration stage, this is a good moment for management and coaching. Provide support, remove obstacles, encourage best practices, and celebrate progress.
Finally, if your providers and staff have reached the Commitment phase, you can reinforce the change by sharing data, communicating success, and identifying new paths for their growth.
For a more detailed approach to these responses, Katie Lawrence can be reached at katie.mm.lawrence@gmail.com.