Making the switch from physical to hybrid care
To successfully transition to hybrid care, physician practices need a cohesive telehealth strategy.

The longer the pandemic wages on, the more it becomes clear: COVID-19 is making telehealth “stick” for physicians and consumers alike.
Four out of five physicians used telehealth during the pandemic, a recent Amwell survey shows, and 92% of physician respondents expect to keep using telehealth even after the pandemic. Consumers, too, find value in virtual care, with over half of respondents saying they will use telehealth more in 2021 than they did before the pandemic.
These trends pave the way for hybrid care—a combination of virtual and in-person care—to become the norm in 2021. Building a successful hybrid model of care requires physicians to tackle big questions around workflow, workforce, technology and the patient experience.
As a physician who started practicing virtually more than eight years ago, I’ve had many years to understand the nuances of remote care. I’ve seen how it can best be implemented into traditional brick and mortar practices to support patients and doctors alike and enable the best care. Here are four ways physicians can lead their practices in making a successful transition to a hybrid care model.
No. 1: Focus on usability.
COVID-19 had a dramatic impact on telehealth use by consumers, with 22% of consumer respondents engaging in a telehealth visit in 2020, up from 8% of respondents in 2019, according to the same Amwell survey shows; recent data suggests telehealth is here to stay.
Already, nearly half of healthcare leader respondents have shifted their organization’s innovation priorities to focus on telehealth and virtual care, according to the Center for Connected Medicine and KLAS’ ‘Top of Mind for Health Systems 2021” report. But accelerating the transition from physical to virtual care requires physician practices to close technology gaps that prevent providers from initiating a smooth, seamless video visit. We saw signs of these gaps in the Amwell survey, where three-quarters of healthcare leaders surveyed said technology challenges presented barriers to video visits in their organization.
To successfully transition to hybrid care, physician practices need a cohesive telehealth strategy—one that is built on a singular platform that emphasizes ease of use, interoperability and flexibility in care delivery. For example, the sudden rush to telehealth during the pandemic meant that providers needed to start seeing patients online quickly, before well-thought-out strategies could be implemented. It also led to a scattershot selection of telehealth technologies. Today, one-in-five physicians uses three or more telehealth platforms, each with its own set of potential issues.
Given that 84% of physicians surveyed are satisfied with at least one telehealth platform, exploring ways to pare down telehealth solutions to a single platform that works well for physicians and consumers alike is one way to smooth telehealth adoption. The easier a platform is to use, the more providers will want to continue using telehealth as at least one means to see their patients.
No. 2: Leverage telehealth for a broader range of use cases.
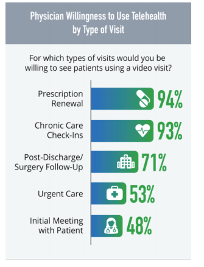
No longer is telehealth primarily a go-to for on-demand urgent care. In 2020, physicians gained a better understanding of how to integrate telehealth into everyday care, such as prescription renewals, chronic care check-ins, and post-surgical follow-ups. Physicians’ openness to using telehealth in a variety of ways could accelerate consumers’ desire for a hybrid care approach. Today, 65% of consumers who haven’t yet tried telehealth say they are “very” or “somewhat” willing to do so, primarily for the convenience (58%) and the ability to gain faster service (47%), the Amwell survey found.
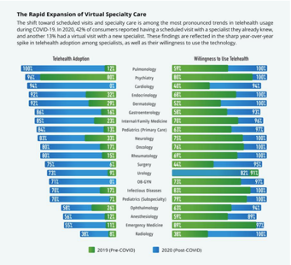
We’re also seeing a rapid expansion of the use of telehealth for specialty care. Pulmonologists, cardiologists, surgeons, and many other specialists reported a sharp increase in telehealth adoption compared to 2019. In high-volume specialties like radiology, cardiology, and surgery, telehealth visits more than doubled in 2020.
The more providers are able to take advantage of telehealth across a variety of use cases, when it’s deemed safe and appropriate, the more telehealth will become a natural part of the care continuum and not seen solely as an urgent care fix. To make the transition, physicians need training not just on “web-side manner,” but also the types of care that can be delivered virtually. Connecting with physicians in your specialty who have experience in telehealth is a good place to start to inform your approach.
No. 3: Consider how to tie together virtual and in-person experiences across the continuum of care.
Hybrid care models connect the in-person elements of care—procedures, labs, imaging, immunizations—with the virtual elements of care, including remote patient monitoring and video consultations with specialists. As physicians build out their hybrid care approach to include a variety of telehealth use cases and devices, they need to think about how they can stitch together both virtual and in-person care to create a seamless experience that fully envelops patients in care when and where it’s needed. Three areas of focus include:
- Workflows. How will physicians incorporate telehealth and other digital tools into existing clinical workflows in a flexible, sustainable way?
- Workforce. How should physician practices optimize staffing models, training and talent to meet the unique needs of hybrid care patients?
- Engagement and experience. How can physicians most effectively engage patients and leverage technology to deliver tightly integrated virtual and in-person experiences?
No. 4: Raise awareness of offerings among consumers.
While COVID-19 drove intense interest in telehealth, many consumers still don’t know if virtual care is available to them personally, whether it’s covered under their insurance, nor how to access it. This makes it incumbent upon physicians and healthcare organizations to educate consumers on both their virtual and in-person options as well as how to access the right care in the right setting at the right time. Such education shouldn’t be limited to older generations: the Amwell survey showed that among Gen-Zers, 30% of respondents who had not yet used telehealth said they were willing to use telehealth, but they didn’t know how to access these services.
If you’re a physician whose practice has just begun to offer telehealth services, it’s important to use a variety of communication methods to educate consumers on availability of virtual care offerings and ways to access telehealth as well whether those visits will be covered by insurance (the vast majority are). Go beyond signage in waiting rooms and exam rooms. During COVID-19, leading physician practices spread the word about telehealth offerings through email campaigns, advertisements on billboards and patient portals, and information on patient billing statements.
Navigating the Future of Hybrid Care
The signs are clear: provider and consumer interest in video visits is evolving from a necessity to a preference. But providing care via one method—solely online or in person—is not sustainable or effective, which is why hybrid care models are where the industry is heading in 2021. For physician practices, however, there are still important gaps in technology, access, and consumer understanding that must be addressed before hybrid care models will truly take off, especially in smaller practices. Focusing on these four areas will better position providers to develop the right strategy for their practice and those they serve.
About the Author
Mia Finkelston, MD, is a physician and senior medical director for Amwell.