Keeping up with regulatory changes during COVID19
Guides on key areas to watch.

These are historic times. As lawyers for primary care physicians we are humbled and grateful for the commitment of our physicians during the COVID-19 pandemic. But the coronavirus is not the only historic factor of these times we are dealing with-the level of regulatory change from federal and state governments is unprecedented. The federal government alone has sent out more than 600 regulatory pronouncements.
In our legal department, we have started to joke that the changes are coming down like rain. We know that the most physicians are also seeing the downpour of changes and are waterlogged trying to make sense of it all.
To help our physician clients, we have curated helpful guides on a couple of key areas to watch. We don’t save lives, but hope this will provide some help to those who do!
Employer Requirements: Layoffs, Sick leave, and Furlough
Several changes relate to managing a work force including the FFCRA, the CARES Act, OSHA requirements and CDC guidelines for personal protective equipment. But in our view, this is not the time to quote chapter and verse. The safety of the working environment has been a difficult and critical issue–covered in headlines and already the subject of litigation. We won’t know how courts rule and how this changes for several months. We recommend providing managers with very tactical practical guidance. We also recommend listening to employees and creating opportunities for them to report concerns. Finally, it is a good idea to track instances of exposure and other related problems. We have created an FAQ that can be customized to your office to provide guidance to your managers.
Staff with suspected or confirmed illness
- Can you send home someone who is sick or may have been exposed?
Employers are required to provide a safe and healthy workplace. If the employer has a reasonable belief that the employee has been exposed to or has contracted coronavirus, the employer may send that employee home to protect the rest of the workforce. The CDC has mandatory requirements for health care workers.
- Do you have a legal duty to pay them for time off?
If you have a PTO policy, you should advise managers of its requirements. If not, employers with less than 500 employees, are required to provide compensation for up to two weeks of sick leave.
- What if they are a brand-new employee?
Lawmakers have relaxed the regulations due to COVID-19. it does not matter if it is a new employee – you still need to pay for up to two weeks of sick leave.
- Do you have to pay them the full rate of pay?
Yes, except when the employee is caring for someone else (e.g. child or family member with COVID-19 diagnosis or symptoms), they are eligible for pay at 2/3 their regular rate, up to $200/day and $2,000 in the aggregate 2-week period.
Staff calling sick or afraid to work
- Can you fire someone afraid to work and refusing to come in.
The answer here is complicated and depends in part on the PPE and procedures you have available. There are limitations on the ability to fire someone if they reasonably believe that the situation at work is an imminent threat to their health. The best course of action here is creating an environment where people can raise their concerns and creating an environment that is as safe as possible.
Work from home – Exceptions apply to health care providers
- Are you required to let your practice/clinic employees work from home, regardless of their position?
If their work is essential to be performed in the office and they have not requested an accommodation you do not need to allow them to work at home.
- Is your practice/clinic required to pay employees who stay home with their children due to school closures?
Employers with fewer than 500 employees are required to compensate their employee at 2/3 their regular rate if they need to stay home with their child(ren) due to COVID-19 school or child care closures.
Return to work
- If someone has been suspected or confirmed positive, what medical evidence should we require to allow them back to work.
If they were exposed with no symptoms- we follow the CDC guidance on the number of days. Otherwise, before returning to work, you have options – you could require a doctor’s note if desired, but you do not need to do this. Legally we should treat similarly situated employees the same. You could as an option to require a doctor’s note to return.
Special Circumstances/Vulnerable employees
- What do we do about staff with conditions that make them vulnerable to illness (pregnancy, chronic illness)?
You don’t need to proactively ask staff or suggest that they are fragile, but if they ask for an accommodation, you may need to provide a reasonable accommodation. This can get complicated. It is preferable if possible, not to simply mandate that they won’t see certain high-risk patients. (Other staff may complain if they are required to do all the high-risk patients and they may have a valid claim.)
Duty to Close
- Is there any duty on employers to close their workplace if a risk of contact with coronavirus is identified?
No. However, employers have a duty to ensure that reasonable care is taken to safeguard the safety and health of employees at work. Reasonable care may be demonstrated by providing extra hand sanitizers, encourage proper hand washing etiquette, and use of a mask and gloves when interacting with patients who may have been exposed or have contracted coronavirus.
OSHA and Worker’s Comp
- Is COVID-19 a recordable employee illness for the purposes of OSHA Logs?
If you have less than 10 employees, these do not apply. If they do apply to your workplace, you should be keeping track of these in your OSHA log. In either case, we recommend keeping close track of this at this time. This is a good idea for lots of reasons. There may even be financial relief available at some point to businesses damaged by this outbreak and this may be a good record to have at that time.
- If your employee contracts COVID-19 at work, will this result in a compensable workers’ compensation claim?
There are some debates on this now, but it is a good assumption that this will be the case.
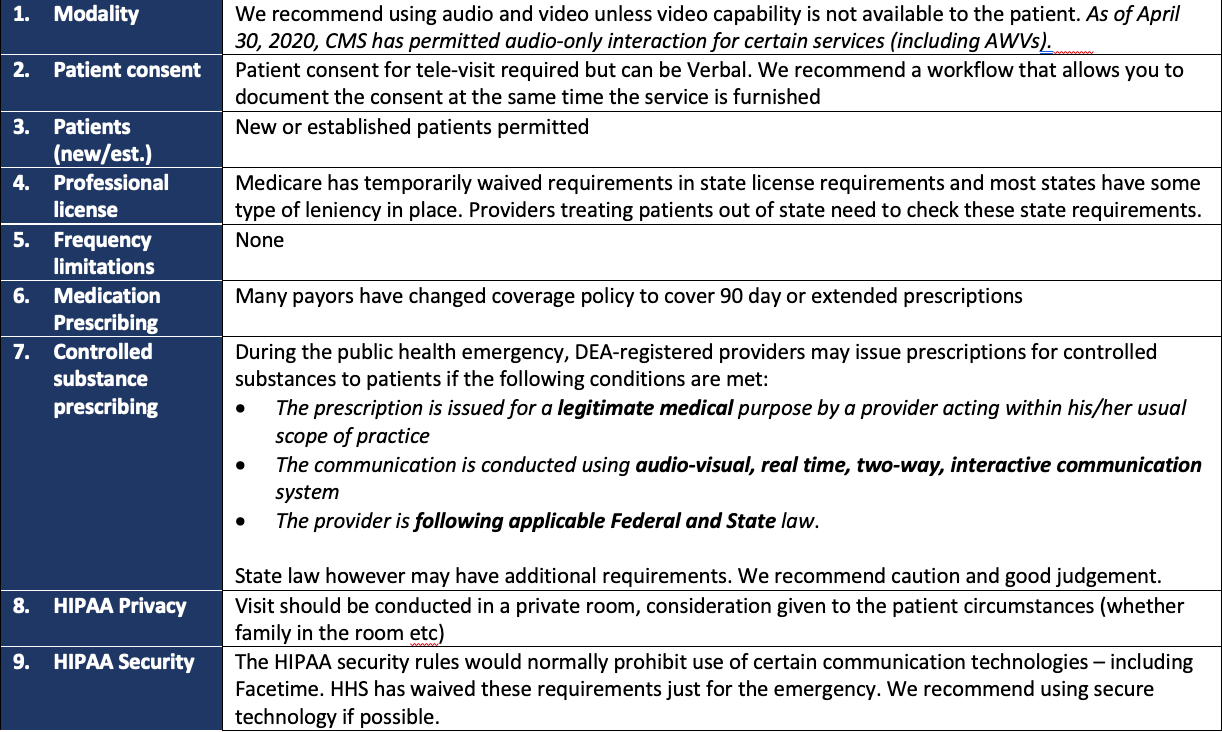
Telemedicine and Remote Monitoring
Most providers have implemented some form of telemedicine option to be able to provide care to their patients during social isolation. The rapid change to provide Medicare payment for telemedicine is viewed by many as important. The details of this change have evolved over time and can be tedious to follow. We have prepared a summary of the most critical points.
Trending: The New Normal for Physicians
Medicare Telemedicine Payment Critical Points; Click to View
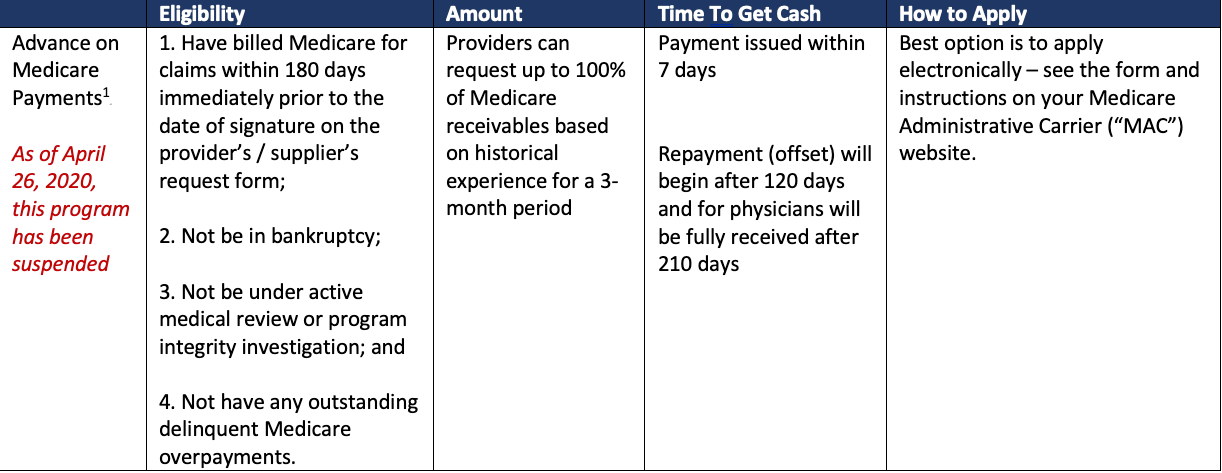
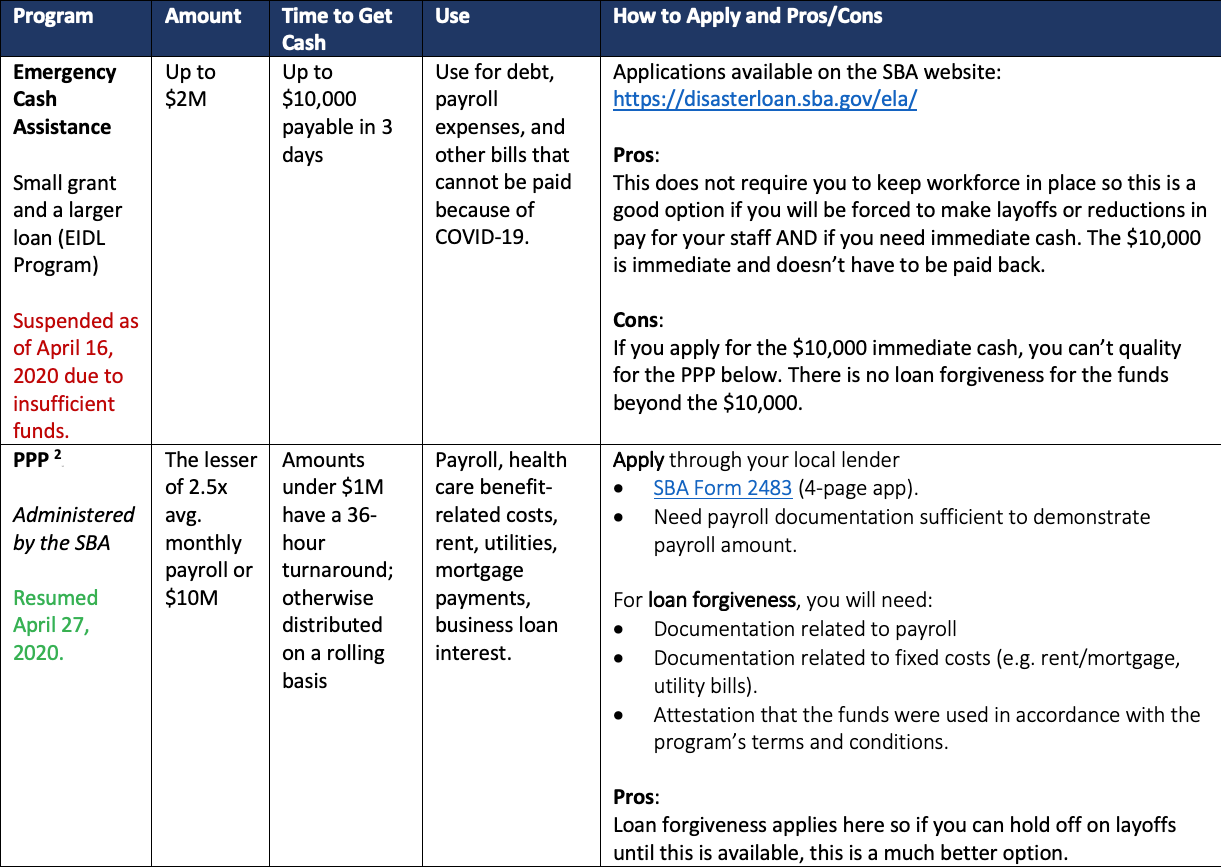
Cash Relief
There are several options available to primary care physicians to weather the financial impact of COVID-19 has caused. It is strongly encouraged to speak with a financial consultant before deciding which program works best for your particular situation. Make sure to keep diligent records of how any funds received are used to ensure compliance with the specific program’s terms and conditions. If you receive more than $150,000 from any federal program related to COVID-19, you are likely obligated to make quarterly reports to HHS and the Pandemic Response Accountability Committee within 10 days following the end of each calendar quarter. A high-level summary of the main cash relief options available to physician practices are explained below.
Cash Relief Options Available to Physician Practices 1; Click to View
Cash Relief Options Available to Physician Practices 2; Click to View
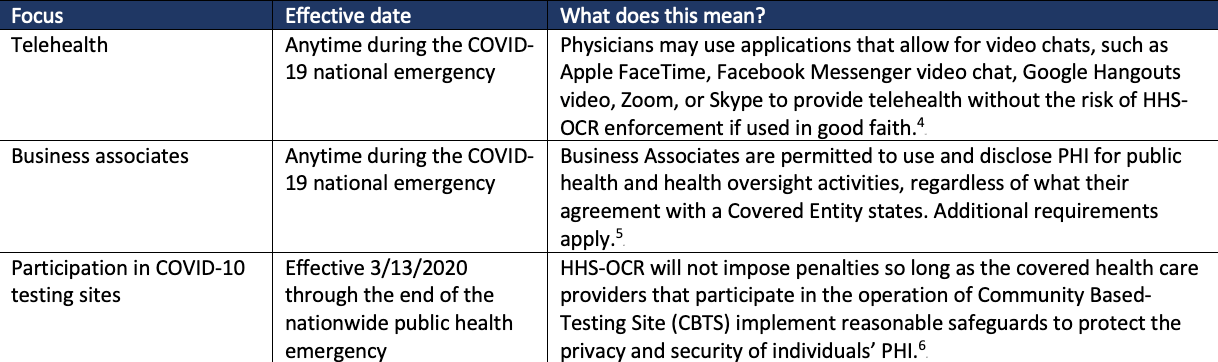
HIPAA
Most of the guidance related to the HIPAA Privacy and Security regulations during the COVID-19 period largely reiterates what the existing law is, such as needing patient consent prior to media access to protected health information (PHI). The changes have occurred as it relates to the HHS-OCR’s enforcement of noncompliance with the regulations, which are described briefly below.
HIPAA HHS-OCR Noncompliance Regulation Updates; Click to View
Practical tip: Also, beware of malicious cyberattacks focused on health care physicians, their practices and health systems, generally. Now more than ever, patients, practitioners, and businesses are relying on virtual technologies making it even more important to make sure the correct cyber protections are in place.
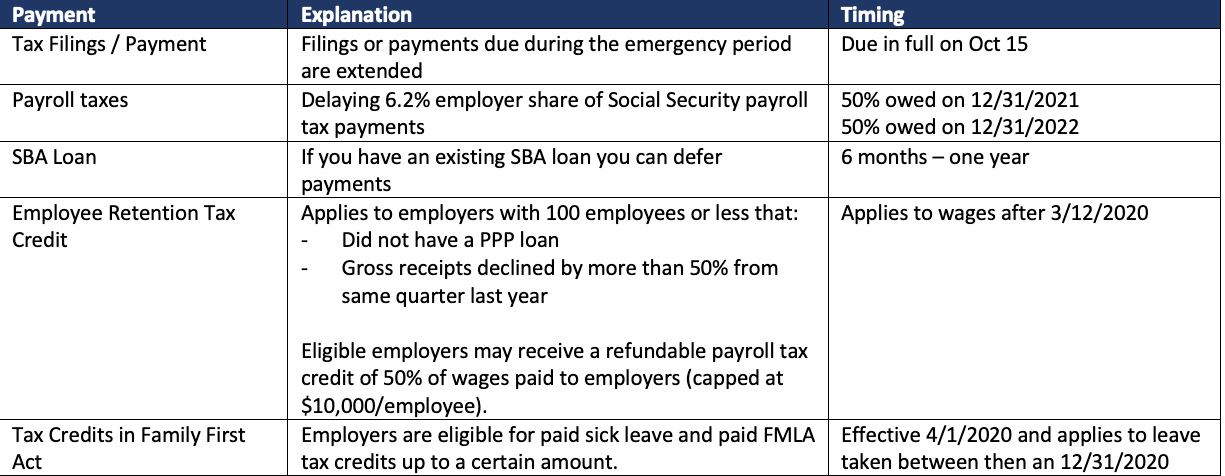
Taxes
The federal government has granted extensions to make certain payments and offered tax credits to reduce the financial burden physician practices are likely experiencing. There are some limitations and other requirements that apply.
Tax Limitations and Explanations; Click to View
Disclosures:
The information included in this article is not all-inclusive and does not constitute legal advice. Also note that the health care regulatory environment is changing daily, and the information included above is only current as of the date it was written.
References:
Paycheck Protection Program, U.S. SMALL BUS. ADMIN., https://www.sba.gov/funding-programs/loans/coronavirus-relief-options/paycheck-protection-program (last visited June 2, 2020).
CARES Act Provider Relief Fund Frequently Asked Questions, U.S. DEPT. HEALTH & HUM. SERVS., https://www.hhs.gov/sites/default/files/provider-relief-fund-general-distribution-faqs.pdf (last visited Jun. 2, 2020).
Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency, U.S. DEPT. HEALTH & HUM. SERVS., https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html (last reviewed Mar. 30, 2020).
Roger T. Severino, Notification of Enforcement Discretion under HIPAA to Allow Uses and Disclosures of Protected Health Information by Business Associates for Public Health and Health Oversight Activities in Response to COVID-19, U.S. DEPT. HEALTH & HUM. SERVS., https://www.hhs.gov/sites/default/files/notification-enforcement-discretion-hipaa.pdf (last visited June 2, 2020).
Roger T. Severino, Notification of Enforcement Discretion under HIPAA to Allow Uses and Disclosures of Protected Health Information by Business Associates for Public Health and Health Oversight Activities in Response to COVID-19, U.S. DEPT. HEALTH & HUM. SERVS., https://www.hhs.gov/sites/default/files/notification-enforcement-discretion-hipaa.pdf (last visited June 2, 2020).
Roger T. Severino, Enforcement Discretion Regarding COVID-19 Community-Based Testing Sites (CBTS) During the COVID-19 Nationwide Public Health Emergency, U.S. DEPT. HEALTH & HUM. SERVS. (April 9, 2020), https://www.hhs.gov/sites/default/files/notification-enforcement-discretion-community-based-testing-sites.pdf.