Build a successful two-way patient engagement model
Patient behavior plays a crucial role in determining health outcomes. In order to improve their health, we must help them get more engaged.
As healthcare professionals, we face so many of our own challenges that it’s easy to forget just how many demands we put on our patients, too. Between coordinating appointments and referrals, shuttling health data from one provider to the next, and filling and managing prescriptions, patients perform countless hours of unpaid, unrecognized, and unsupported work.
Being sick in America can feel like a full-time job. Too many patients who don’t know what resources exist to help them essentially stop showing up to their doctors’ offices. In turn, those patients are not getting the care they deserve-and need-to improve their health overall.
Research shows that patients who are not engaged are three times more likely to have unmet medical needs and twice as likely to defer necessary care. When it comes to accessing electronic health records (EHRs), an Accenture survey found that 84 percent of patients believe they should have access to their health records. And when it comes to scheduling, American patients are far less likely to secure a same-day doctor’s appointment than patients in most other developed countries. The longer patients have to wait for an appointment, the less likely they are to actually show up.
Given the significant role patient behavior plays in determining health outcomes, we must help patients succeed. Unfortunately, our industry’s current technology simply doesn’t suffice. We won’t realize the benefits of improved patient engagement until we put processes in place to reach patients where they are to actively make their lives easier.
To truly support patients in fulfilling their responsibility as patients, providers must recognize that the traditional perspective of how to interact with patients-during scheduled visits, in the office, within the confines of four clinical walls-is outdated. Instead, let’s take a page out of the retail industry’s playbook. Rather than waiting for patients to come through the door, let’s build more channels to engage them wherever they are and give them accessible and actionable resources.
Some of these channels require new infrastructure such as urgent care clinics and home health services. The underlying technology of this new future will be comprehensive and legible patient portals that serve as a connector for patients and providers. These allow providers to reach outside their offices and into the homes and communities they serve. For patients, portals are the most effective and inclusive tool to help them participate in their own care: sharing information securely, scheduling appointments, messaging providers, managing bills, accessing education materials, and more.
Studies show that when patients succeed, we all succeed. When athenahealth researchers reviewed data from about 400 practices, we found a strong link between portal adoption and clinical performance. For example, practices in the bottom 20 percent in terms of portal adoption are generally below our network-wide average in controlling HbA1c and a host of other quality metrics, including hypertension control and preventive cancer screenings. Conversely, the top 20 percent of portal adopters are leaders in controlling diabetes and other quality indicators.
Portals also have a documented positive effect on the bottom line. Recent studies have found that physician practices with a high portal usage could expect annual savings through online billing inquiries, electronic delivery of lab results, and self-scheduled visits. What’s more, athenahealth clients have found portal adoption to be highly correlated with patient loyalty and pay yield-key drivers of financial success.
So, what’s the holdup?
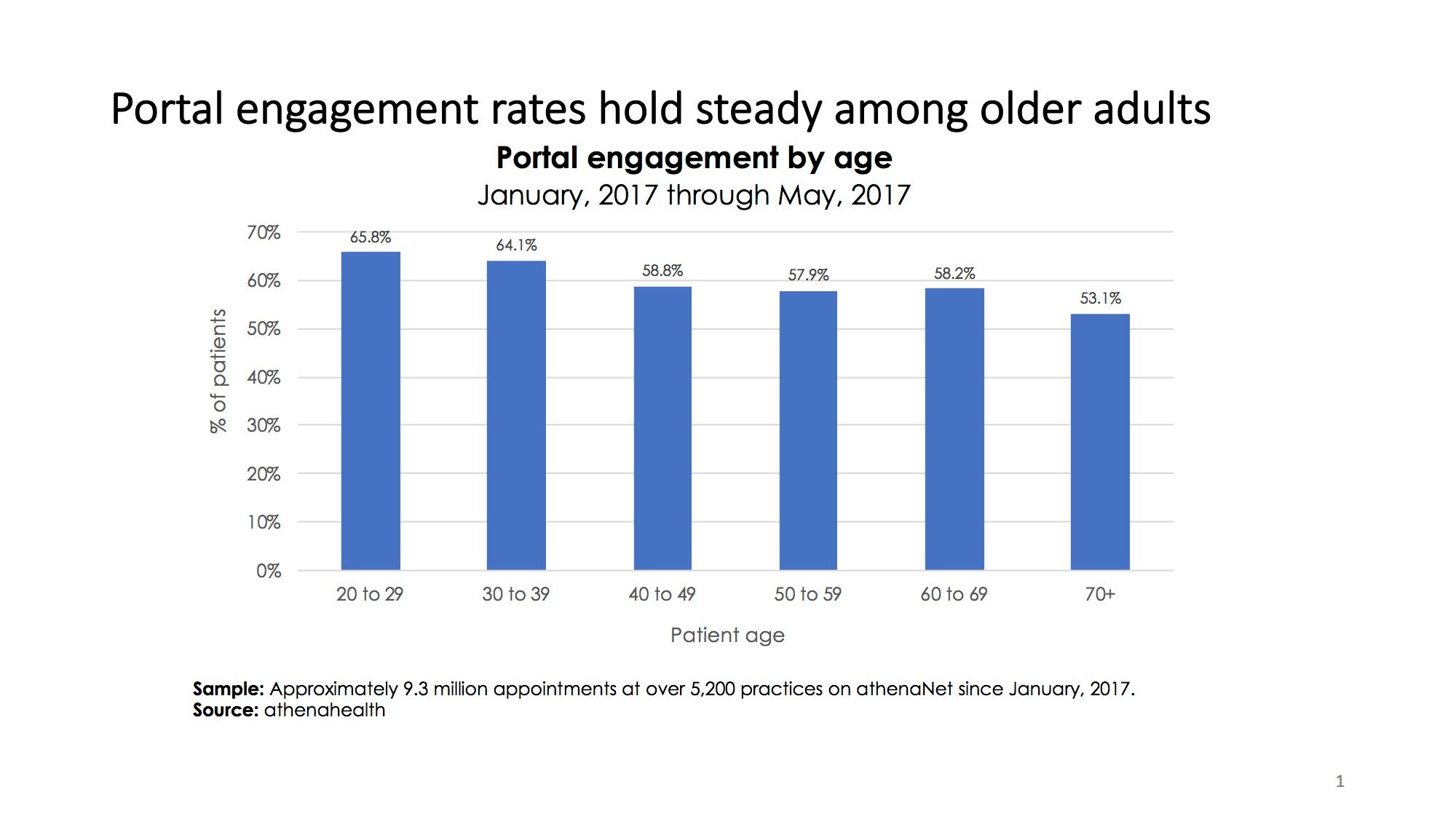
Several myths are preventing widespread portal adoption throughout the industry. This first is that portals are only popular among millennials. Not true. Athenahealth data has found that patients in their 60s engaged with their provider’s portal at the same rates as did patients in their 40s and 50s-about 58 percent. That’s only slightly less than patients in their 30s, of whom 64 percent had engaged with their portal.
The second myth is that boosting portal adoption doesn’t pay off tangibly or in the near term. Our findings and real-world examples suggest otherwise. Take Carolina Health Specialists, a multispecialty group based in Myrtle Beach, S.C. After a short rollout, the practice now has 65 percent of its patients using the portal, an adoption rate the group believes explains two other statistics that are well above the benchmark: an 82 percent patient retention rate and 3 percent no-show rate. The group uses aggressive outreach and gamification methods to explain the benefits of the portal and make using it a “sticky” habit. An in-house team of trained call center representatives is available to help troubleshoot for patients. The staff reply in a timely manner to patient messages, and contests are held between nonclinical staff over who can sign up the most patients to the portal.
Perhaps most importantly, the practice also views the portal as a two-way channel. Patients use the portal to schedule appointments, including same-day and after-hours options; review health information and care plans; and view lab results.
For its part, Carolina Health Specialists regularly pushes out humorous reminders for screenings and vaccinations, such as a photo of a sick basset hound with a thermometer under its lip. The practice also sends reminders to patients about their responsibilities, including how they can pay at the time of appointments. Last summer, the practice supplemented this patient education with a flat $35 no-show fee. Taken together, these measures led to a 50 percent drop in missed appointments.
In healthcare, there is immense opportunity using portals and other technology to provide patients with the information, visibility, and feedback they need to achieve good health. Technology can’t do everything, of course. Patients still need to embrace behavior change and take accountability for their own care. But, technology can make their job easier and ultimately create meaningful outcomes on both sides of the care experience.
Kevin Ban, MD, is chief medical officer for athenahealth. Previously, he was the chief medical officer at Beth Israel Deaconess Hospital-Needham in Massachusetts.