Being Proactive to Take on Value-Based Care
By: Gregory Corradino, MD MBA Pay-for-performance is coming. Physicians need to be proactive when dealing with this major change.
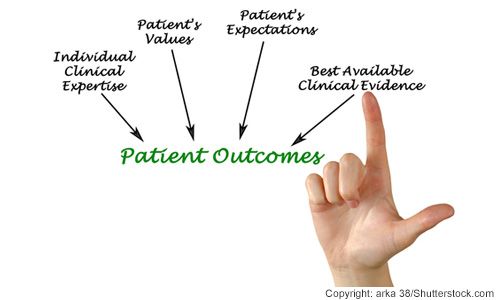
Recently, I attended a leadership seminar on “Value-Based Purchasing,” Medicare’s reworded attempt to improve quality and efficiency in medicine. The original title of this program was “Pay for Performance.” In this session, we learned that Medicare payments will be increasingly tied to “performance” measures such as cost, patient satisfaction, and “outcomes”. Sound confusing? I think it’s intended to be.
In any case, what can one do? Well, the way I approach this situation is the way I approach problems in surgery: I ask myself, what is one thing I can do RIGHT NOW to make this situation better? (Of course, I don't do this out loud). The point is this: As individual physicians, we cannot turn away to the tsunami of changes that big government and big insurance companies are bringing our way, but we can change how we act in response.
One of Steven Covey’s, “Seven Habits of Highly Effective People” is to “Be Proactive”. Notwithstanding the fact that we are “reacting” to these changes in the medical climate, what does this mean to us? First, it means we need to accept these changes as fact because as individuals, we cannot change them. Second, we should look for ways in which we can improve things over which we do have control. In this case, since patient satisfaction and costs are two measures being watched, we might as well start with them.
Let’s take “patient satisfaction” as an example, and put aside the argument for the time being that this is an inaccurate measure of quality (in one study it was found that “patient satisfaction” had an inverse correlation to mortality). Here is the process I take when looking at this problem:
• What is being measured?
• How do I rate?
• Where am I lacking?
• How can I improve?
• In this case, the following “doctor items” are being measured:
-Were you treated with courtesy and respect?
-Did the doctor listen carefully to you?
-Were things explained in a way you could understand?
Now, is there any reason we should object to these questions? I think most physicians would strive to do well on any of these measures and if we approach each patient interaction with these goals, we would likely improve our scores (and maybe be a better doctor in the process). The same process can be used to deal with the other measures being examined by Medicare (and other insurance companies).
Viewing change in such a proactive way has helped me adjust in a much more constructive way during my career, and I am convinced it will help anyone who takes this approach.