Ambulatory Care Exposures Result in High Claims Frequency and Severity
One of the most useful ways for ambulatory medical practices to determine malpractice risk is to look at the data.
One of the most useful ways for ambulatory medical practices to determine malpractice risk is to look at the data; that’s what major national malpractice insurance provider Coverys did. They analyzed 6,058 claims that were closed between 2019 and 2023 to determine the most important risks that physicians and other providers need to be aware of to protect themselves from adverse events and reduce their exposure to liability.
Physicians Practice sat down with Marlene Icenhower, JD, BSN, CPHRM, and Heidi McCoy, MSN, BSN, RN, CPHRM, CPPS, two experts from Coverys, to discuss what they found in the data and takeaways for ambulatory care providers. The following discussion was edited for length, clarity, and style.
Physicians Practice: What are the primary risk factors for medical malpractice claims in ambulatory care?
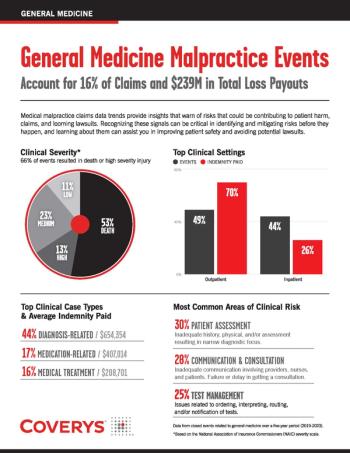
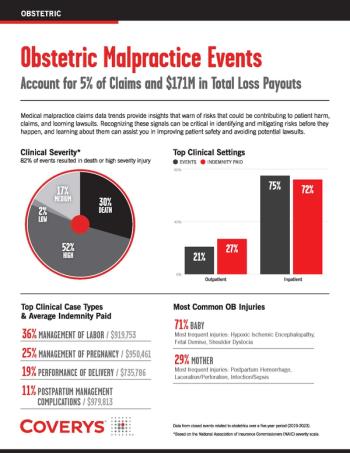
Icenhower: Coverys is one of the biggest providers of medical malpractice insurance in the nation, and for the past 10 years, we've been analyzing our claims data to look at what areas in medicine expose organizations to the most risk. Our data analysts reviewed 6,058 claims that were closed from 2019 to 2023 to see how many of them originated in the ambulatory care setting and how that stacked up to other areas in healthcare organizations. We found that around 25%, or 1,453 of those claims, originated in the office setting, and about 26% of all indemnity paid across the entire company was attributable to those office-based claims. That's more than any other practice setting. I think that data is really interesting because it is not what people expect. I think if you got a bunch of administrators or risk managers together and asked them what departments in their organizations expose them to the most risk, they would probably say ED or labor and delivery. And that is where many organizations focus their risk management efforts—in the ED and Labor & Delivery Unit. But based on our data, maybe they should be focusing their efforts across the street in the clinics. The vast majority of claims in ambulatory care are diagnosis-related, and that's what we see across the board in all other practice areas — the majority of claims are diagnosis-related. The providers most often involved in these claims are primary care providers: family medicine, internal medicine, and geriatric providers. So, these claims are arising out of every day, routine healthcare encounters.
Physicians Practice: How can medical practices in this sector proactively reduce their liability?
McCoy: The key to reducing your liability is implementing a robust risk management program that includes solid policies and procedures, processes, and audits to ensure policies and procedures are being followed, along with providing ongoing education to your teams. Staff need to understand the rationale behind what they are doing and how it contributes to enhancing patient safety and mitigating risk in their care setting. I really want to discuss the specific strategies that can be implemented to improve diagnostic accuracy in order to minimize claims. When we analyzed all of these claims together, we identified that major risks fell into three buckets:
- Clinical decision-making.
- Refining clinical systems.
- Managing patient engagement.
Those were the top three risk management allegations that we found when we looked at ambulatory care claims. Let's talk about each risk area.
Risk 1: Clinical decision-making
When it comes to clinical decision-making, it's important to ensure clinical decision support tools are available for our providers and they are in a centralized location in the EHR for ease of access. We must understand cognitive biases and how those play a role when it comes to clinical decision-making for patients. The data revealed a gap when it comes to having adequate history and physical exams complete. When you think about it, if you don't have an adequate patient evaluation, there's a cascade effect that occurs; it’s difficult to identify appropriate diagnostic tests and follow up if you don't have solid data to support and move those decisions forward. Having a policy that includes documentation of specific elements of that patient and family history and physical exam is extremely important, as is ensuring the information is updated on every visit and available in a centralized location so providers can find it.
For example, one thing we found is that there is a failure to diagnose cancer in these settings, particularly prostate, lung, breast, and colon cancer. During the height of the COVID pandemic, many patients did not receive routine preventative health screening exams. The American Cancer Society is anticipating more than 2 million new cancer diagnoses this year, which is a record high, and this includes a growing trend of cancer diagnoses among adults under the age of 50. We must be aware of and follow the updates to cancer screening guidelines and keep this information updated with appropriate triggers in the EHR. Also, make sure you document informed refusal for patients who decline preventative health screenings. The medical record must reflect why the screening was declined and that the patient understands the risks of not having this done. As a reminder, perform periodic auditing to ensure the history and physical exams are being completed and preventative screening guidelines are being followed per policy and use that information in your patient safety improvement plan.
Risk 2: Clinical systems
The second highest category of risk is clinical systems issues. What we found in the closed claims data is that most often the errors that occurred were related to faulty organization systems rather than the fault of one individual. There are things we can do to help mitigate these types of risks, such as refining processes for following up on test results, including critical results and incidental findings, and finally, being aware of diffused responsibility. Diffused responsibility occurs when one person fails to act because they assume that someone else will take action or should take action. This is a common finding in diagnostic error cases—especially ones involving the failure to follow up on incidental findings. Effective communication between providers is essential. You can set your providers up for success by tightening radiology and lab processes to make sure that incidental findings are communicated effectively and that handoffs are being done between providers. Finally, guidance can be provided by risk managers as to when direct or synchronous communication must be used and when asynchronous (indirect) communication can be used. Critical information should always be conveyed by direct communication, so pick up the phone and have those conversations.
Risk 3: Managing patient behaviors
The third area of risk that contributes to diagnostic error claims is behavioral issues. In this context, we are talking about setting clear expectations, so patients are well-informed about the importance of engagement as a partner in the process. It's really important that patients understand not only their rights but their responsibilities as well. Providers and care teams need to make every effort to help them understand what is expected of them within the healthcare system and within your practice, and they should know what to expect from you. It’s important to set expectations up front and provide clear instructions. Remember that patients can see your clinical notes now, so it's important to be kind, be positive, and use language that patients understand. Finally, it's valuable to understand the patient's goals and what their expectations around their treatments are, along with their priorities, because they're not always aligned with what a healthcare provider thinks is best. So be sure you understand where your patients are coming from and their healthcare goals.
Physicians Practice: What role does effective documentation play in preventing malpractice lawsuits?
Icenhower: Documentation is the cornerstone of healthcare; it's the primary way that the care team communicates clinical information to each other. It's also the way that we communicate with patients about their health and their responsibilities and obligations. So, as with everything in the medical legal world, documentation is key. As Heidi said, most of these diagnostic error cases involve a missed or delayed diagnosis of cancer. So, it's really important that when providers are documenting, they're thoroughly documenting the differential diagnosis, the patient's history and physical exam, family history of cancer, and the communication of test results to patients. All of these little pieces of information can become really important in the context of a lawsuit. In short, documentation is the best evidence of the care that you provided to the patient, so it's important to not shortcut the process.
Physicians Practice: How can practices manage patient expectations and communication to mitigate the risk of misunderstandings?
McCoy: As I mentioned earlier, patients should have a clear understanding of what they can expect from the practice, but also what their rights and responsibilities are for their own health. When we review the underlying causes of claims, we often find issues related to patients not following up on recommended tests or treatments. These issues arise when patients aren’t clear about things like how medication refills are managed, how appointments are scheduled, showing up for appointments, their role in preventive health screenings, and things like that. Your patients really need to understand the operations of the practice and how to best navigate that to get their needs met. Being specific is crucial, and patients need to understand what behaviors are not OK.
As Marlene explained, documentation is key in order to convey clinical information and to support the care you provided to the patient. But you also have to document so that the patient understands the information when they go in the patient portal to view their medical record. Make sure that you are clearly documenting the education you provided to the patient and the patient understanding of the information that you provided in order to set these expectations. Many providers use a well-crafted patient brochure and signage for patient education. And when communicating with patients about expectations, be sure to use a teach back, so they can better understand the expectations.
Physicians Practice: Why are diagnosis-related claims so prevalent in medical malpractice cases?
Icenhower: Heidi talked about how one of the chief risk factors that we see in these claims is clinical decision-making—essentially the process that providers use to come to a diagnosis. The diagnostic process is a really complex one. Some of the steps are analytical and data-driven, like getting an EKG, taking blood pressure, and so on. That's the “science” part of medicine. Part of the process, on the other hand, is intuitive—it is based on experience, context, and reasoning. That's the “art” part of medicine.
All along the way during this diagnostic journey are opportunities for error. Sometimes claims begin with cognitive bias that may be paired with a narrow diagnostic focus, which is like tunnel vision, where the diagnostician focuses on their presumed diagnosis to the exclusion of other things. Sometimes diagnostic errors occur as a result of inadequate or inappropriate history taking. The failure to order appropriate diagnostic tests or obtain specialty consults or referrals can also be a factor. Any of these things alone or in combination can contribute to diagnostic error.
The thing that makes diagnostic error such a challenge, in the ambulatory care setting at least, is that it can be hard to detect. In other words, when you're looking at your risk or incident data, there are some things that stand out. For example, medication errors are easy to spot. Patient falls are obvious. They reveal themselves quickly. But diagnostic error may take time, sometimes years, to be discovered, and feedback about the misdiagnosis is not always received. Patients may go to another provider who discovers the misdiagnosis, and the feedback loop is never closed. The point is, diagnostic error is often insidious, and I think that's what makes it so dangerous. That's why being aware of the potential for diagnostic error is really important—so that you can refine your clinical systems, understand clinical judgment issues, and head off patient behavioral issues before they result in claims.
Coverys insurance products issued by Medical Professional Mutual Insurance Company and its insurance subsidiaries, Boston, MA.
This article is for informational purposes only and may not reflect the most current legal or medical developments. This informational material is not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.
Newsletter
Optimize your practice with the Physicians Practice newsletter, offering management pearls, leadership tips, and business strategies tailored for practice administrators and physicians of any specialty.