2022 PFS Impact on Telehealth and Care Management: Initial impressions
What the new physician fee schedule may mean for your practice.

Early this month, the Centers for Medicare & Medicaid Services issued its eagerly awaited 2022 Physician Fee Schedule (PFS) final rule. I recently presented a webinar on the subject, focusing on some of the most significant developments concerning telehealth and care management. The questions and comments I received from providers and healthcare professionals during the program were relatively focused on a few specific aspects of the new rule. Using that feedback as a guide for what is top of mind for providers, below is a summary of the big takeaways on how the final rule impacts telehealth and care management.
Chronic care management is a big winner
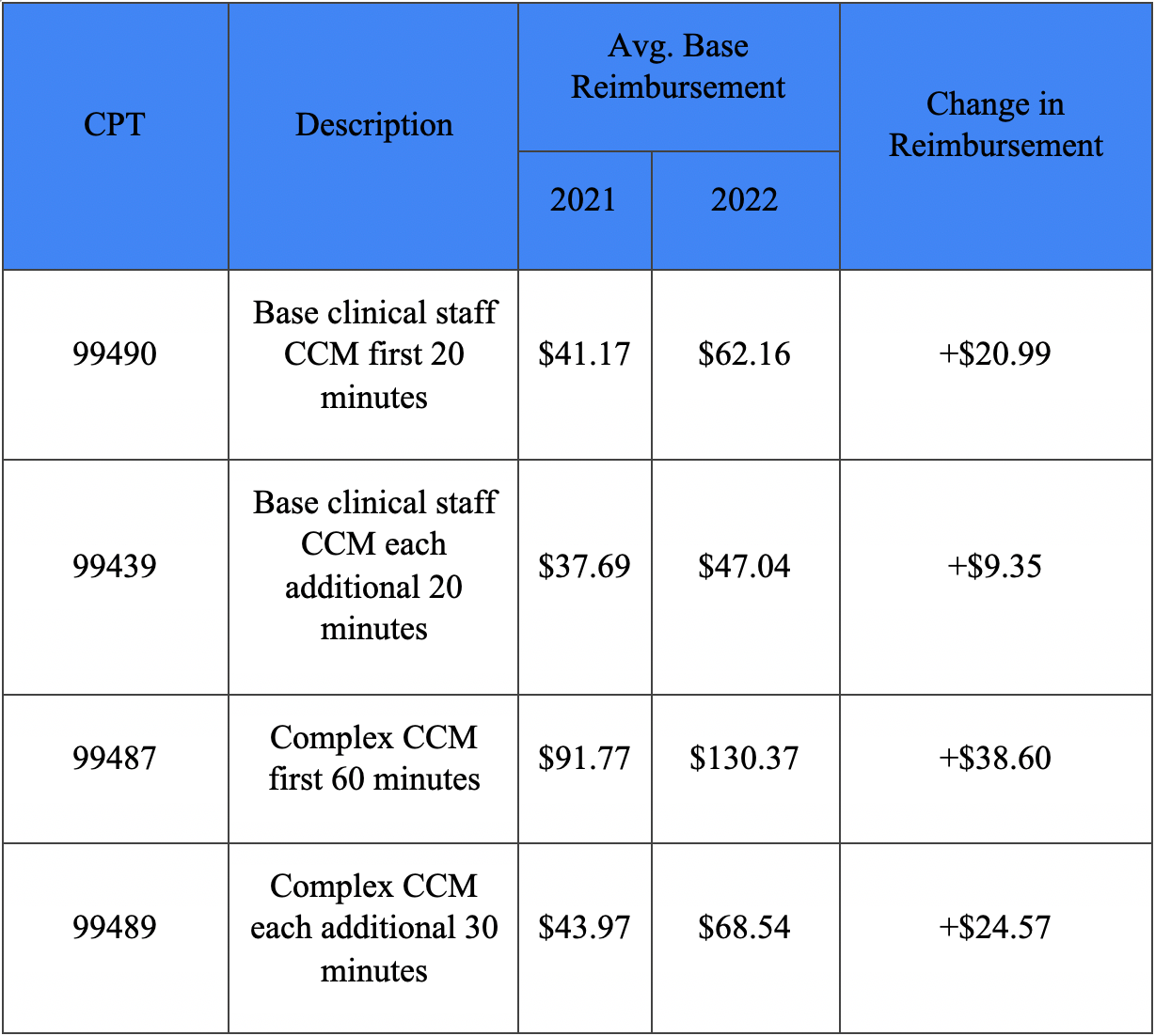
Chronic care management (CCM), and with it complex chronic care management (CCCM) and principal care management (PCM), further cemented itself as one of the most lucrative Medicare programs and is a program all practices should look into offering for patients in 2022 and beyond. The 2022 proposed rule indicated that CMS was planning to throw its weight behind CCM, and that's exactly what it did in the final rule. Most significantly, CMS finalized a significant increase in reimbursement for some of the CCM and CCCM CPT codes. Highlights include the following:
CMS also finalized the addition of five new CCM and PCM CPT codes:
- CPT 99437 — CCM services each additional 30 minutes by a physician or other qualified healthcare professional, per calendar month (List separately in addition to code for primary procedure)
- CPT 99424 — PCM services for a single high-risk disease first 30 minutes provided personally by a physician or other qualified healthcare professional, per calendar month
- CPT 99425 — PCM services for a single high-risk disease each additional 30 minutes provided personally by a physician or other qualified healthcare professional, per calendar month (List separately in addition to code for primary procedure
- CPT 99426 — PCM, for a single high-risk disease first 30 minutes of clinical staff time directed by physician or other qualified healthcare professional, per calendar month
- CPT 99427 — PCM services, for a single high-risk disease each additional 30 minutes of clinical staff time directed by a physician or other qualified healthcare professional, per calendar month (List separately in addition to code for primary procedure)
"Direct supervision" via telehealth remains up in the air
CMS declined to act on remote direct supervision of clinical staff providing "incident to" services. For now, the agency is not making permanent the temporary exception that permits the virtual presence of the supervising physician or practitioner using telehealth. This form of direct supervision is permitted through the later of the end of the calendar year in which the COVID-19 public health emergency (PHE) ends or Dec. 31, 2021. Considering the current state of the PHE, direct supervision via telehealth is likely to remain approved through at least 2022.
What's the significance of delaying a final decision on direct supervision via telehealth for service providers? Many services that can be furnished by clinical staff, including the Medicare annual wellness visit (AWV) and other preventive services, can continue to be performed by agents of a provider while those agents are not physically present in the provider's office. Throughout the PHE, we have seen an increase in clinical call centers contracting with physicians to provide such services to a larger percentage of the population than was receiving those services previously.
In the final rule, Medicare stated that it may review the topic in future rulemaking. Although it is unlikely that any more changes will occur in 2022, it is worth keeping a long-term eye on the remote direct supervision requirement and on the list of services that only require general supervision. There has been a large push to decentralize non-physician visits, and it will be interesting to see how Medicare responds.
Category 3 services are extended and grows a bit
In the 2021 Medicare PFS final rule, CMS created a third category (i.e., Category 3) of criteria for adding services to the Medicare telehealth services list on a temporary basis following the end of COVID-19 pandemic. With the 2022 final rule, CMS has extended the timeframe for reimbursement of this temporary category of telehealth services until the end of 2023 with the stated goal of collecting data to see if these services should be allowable via telehealth after the PHE concludes.
CMS added four new outpatient cardiac rehabilitation codes on a Category 3 basis. They are as follows:
- CPT 93797 — Physician or other qualified healthcare professional services for outpatient cardiac rehabilitation; without continuous ECG monitoring (per session)
- CPT 93798 — (Physician or other qualified healthcare professional services for outpatient cardiac rehabilitation; with continuous ECG monitoring (per session)
- HCPCS G0422 — Intensive cardiac rehabilitation; with or without continuous ecg monitoring with exercise, per session)
- HCPCS G0423 — Intensive cardiac rehabilitation; with or without continuous ecg monitoring; without exercise, per session)
Remote therapeutic monitoring remains in a state of flux
In the 2022 proposed rule, CMS devoted attention to remote therapeutic monitoring (RTM), which is different from remote patient/physiologic monitoring (RPM). It was a topic that largely remained under the radar prior to the release of the proposed rule as many details about RTM remained unclear. The final rule further defines RTM but still leaves questions unanswered.
Most significantly, CMS finalized five RTM CPT general medicine codes. As such, they can be billed by physicians and other qualified healthcare professionals who cannot independently order and bill for E/M services (e.g., physiatrists, nurse practitioners, physical therapists. In addition, the codes are designated as "sometimes therapy" codes, which CMS notes to mean that the services can be billed outside a therapy plan of care by a physician and certain nonphysician practitioners (NPPs)when appropriate. The codes are as follows:
- CPT 98975 — Remote therapeutic monitoring (eg, respiratory system status, musculoskeletal system status, therapy adherence, therapy response); initial set-up and patient education on use of equipment
- CPT 98976 — Remote therapeutic monitoring (eg, respiratory system status, musculoskeletal system status, therapy adherence, therapy response); device(s) supply with scheduled (eg, daily) recording(s) and/or programmed alert(s) transmission to monitor respiratory system, each 30 days
- CPT 98977 — Remote therapeutic monitoring (eg, respiratory system status, musculoskeletal system status, therapy adherence, therapy response); device(s) supply with scheduled (eg, daily) recording(s) and/or programmed alert(s) transmission to monitor musculoskeletal system, each 30 days
- CPT 98980 — Remote therapeutic monitoring treatment, physician/other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; first 20 minutes
- CPT 98981 — Remote therapeutic monitoring treatment, physician/other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; each additional 20 minutes
RTM coverage will have major limitations in 2022 given how these initial CPT codes are written. The device supply codes are currently limited to just respiratory or musculoskeletal system monitoring. RTM management time must be furnished by the actual billing practitioner, not clinical staff under supervision. CMS projects primary billers of RTM will be physical therapists, physician assistants, and clinical social workers
Longer virtual check-ins get the permanent green light
Finally, the 2022 final rule permanently adopted coding and payment for the longer virtual check-in service described by HCPCS G2252 — Brief communication technology-based service, e.g., virtual check-in service, by a physician or other qualified healthcare professional who can report evaluation and management services, provided to an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 11–20 minutes of medical discussion.
Virtual check-ins are considered a "Communications Technology-Based Services" (CTBS) by Medicare. These are services that use telehealth technology but do not directly replace in-person services, which allow Medicare to provide coverage for them outside of the restrictive legislation that surrounds telemedicine. The virtual check-in code covers extended services delivered via synchronous communication technology and includes audio-only solutions, gives practices another option to HCPCS G2012, which only covered "5-10 minutes of medical discussion."
Steps for practices to consider
The new payment structure that comes out of the final rules emphasizes the need for comprehensive remote patient care management programs. While the rule does include a decrease in RPM device-supply reimbursement, the increase in reimbursement for care management time spent makes up for the disappointing device reimbursement development.
Practices would be well-served to see where they can dual enroll patients and provide CCM and RPM simultaneously. So, if you're considering enrolling a patient in CCM, adding an RPM device when it provides clinical value is still worthwhile from a reimbursement perspective. When a patient has an RPM device billable under CPT 99454, you can still count care management time spent under CPT 99490 when the other requirements for CCM are met.
The broader takeaway: Try to create a comprehensive remote patient care management program that supports patients utilizing a mix of the care management services that are best suited to their specific conditions and risks. This means leveraging a mix of CCM, PCM, behavioral health-integrated CCM, RPM, virtual check-ins, and other, non-recurring CTBS codes as needed.
About the Author
Daniel Tashnek is the co-founder of Prevounce Health, a healthcare software company that simplifies the provision of preventive medical services, chronic care management and remote patient management. Daniel is also a practicing healthcare attorney specializing in regulatory compliance, reimbursement, scope of practice, and patient care issues.