2010 Fee Schedule Survey
Our 2010 Fee Schedule Survey indicates that with commercial payments narrowly keeping pace with Medicare, practices need to get paid more for the work already being done.
"Data, data, data. That's the key."
So says Deron Schriver, executive administrator of The Women's Healthcare Group in York, Pa. In an atmosphere of fluctuating reimbursements, shifting patient insurance coverage, and the uncertain impact of health reform on private practice, quality data to inform decision making is more important than ever, Schriver says.
When he joined the 6-physician OB/GYN practice nearly five years ago, he found that it was being underpaid by most payers, compared to the going rate at the time. "I think our payers really knew they were getting a good deal with what we had in place," he says.
But after a little cleanup and some reorganization, Schriver says the practice is caught up, has its data readily available and constantly monitored, and there has definitely been a reaction from payers.
"I've noticed it is getting difficult each year to get the increases we are looking for," he says. "There is a lot of push back and a lot of offers and counteroffers taking place in our negotiations."
But Schriver notes that as far as reimbursements, the practice is "very pleased" knowing "it has been a little tough out there."
"I'd say the rates we are getting are keeping us financially strong, regardless of what we are seeing with the economy, so we are pleased about that," he adds. "However, we are noticing the environment out there is getting more difficult from a reimbursement standpoint."
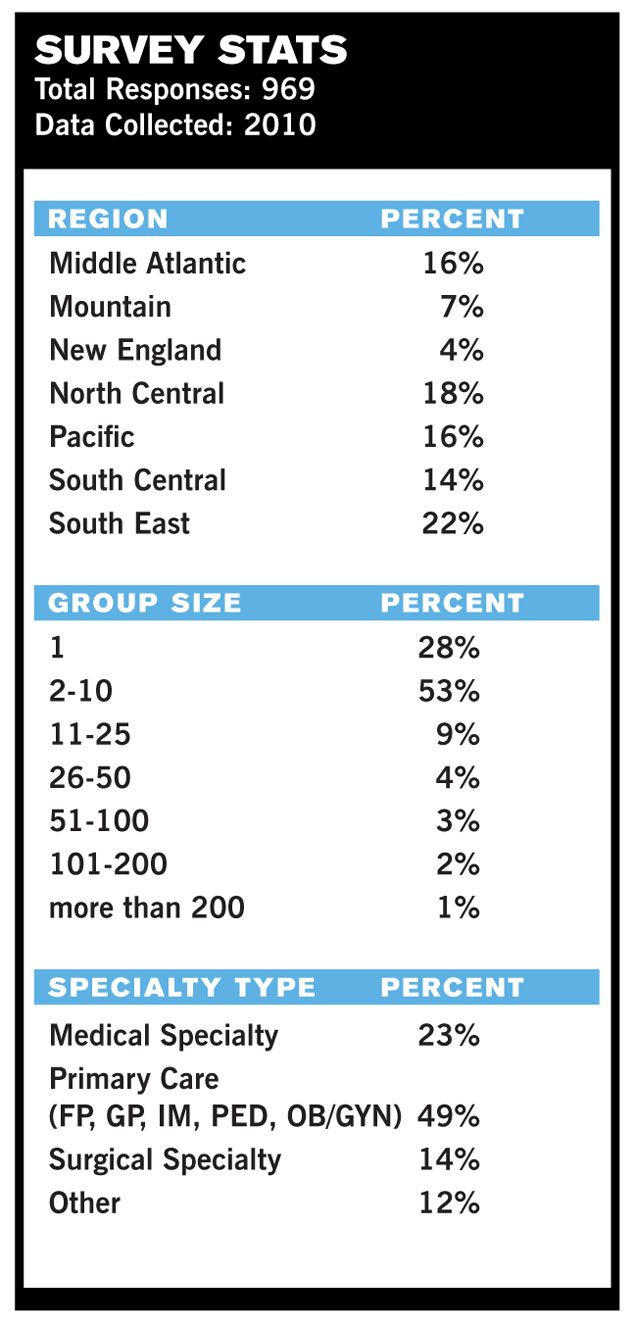
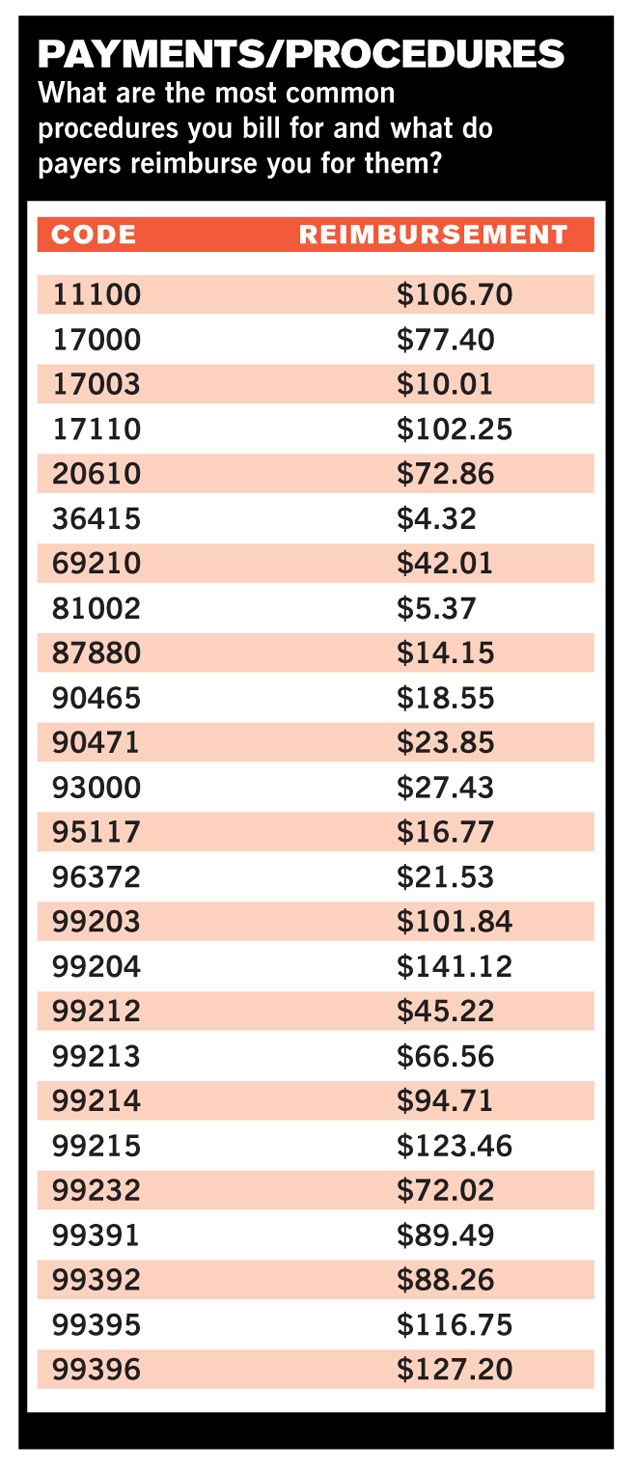
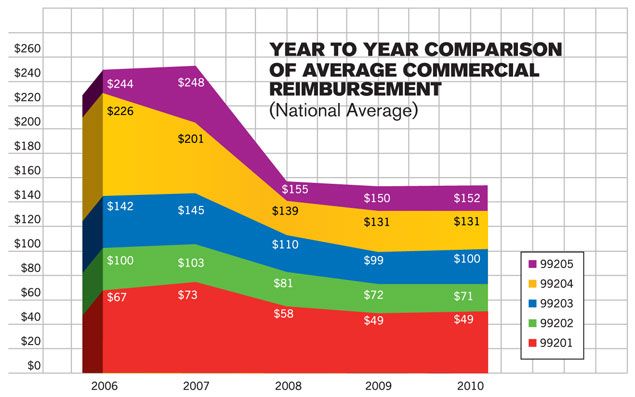
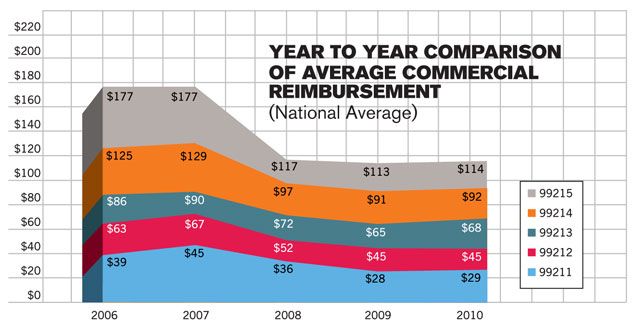
This is evident in our 2010 Fee Survey Schedule. Looking at national averages for commercial reimbursement for new and existing patient visits, the average increase in payments by commercial payers is only 1.4 percent from the prior year. Government reimbursement continues to lag commercial rates, although by narrower margins.
The complete data are found on the following pages, along with some analysis. More important, though, is advice from the experts on how to put your practice ahead of the average.
For the most part, commercial payers are still above national Medicare reimbursement rates, except when it comes to longer visits with patients. The 99204, 99205, 99214, and 99215 visits are all being reimbursed, on average, 18 percent below Medicare, with the 99205 a whopping 28 percent lower. The 99213 midlevel established office visit is reimbursed by commercial payers at $68.27, up 4.1 percent from 2009 - the biggest leap among all E&M codes - and slightly higher than Medicare's $66.74 payment, which itself is up 8.1 percent from last year.
In fact, all Medicare reimbursement rates for E&M codes are up an average of 7.4 percent. Congress and the president avoided a double-digit Medicare cut in June, replacing it with a modest increase in average rates of 2.2 percent. But draconian cuts in Medicare seem to be on the table at all times, and Congress was wrestling with a prospective cut of 21 percent as this issue was going to press.
So with the likelihood that whatever is done at the federal level will be mirrored among private payers, it is more important than ever that practices look hard at the data when it comes to the dollars coming from three key sources: commercial payers, the government, and patients.
You can find tips and advice on how to work with patients on what they owe by reading "Getting Patients to Pay."
Here's some help in getting paid more for the work you are already doing at your practice and some things you might be able to tweak to boost revenue.
Get in the mix
Part of Schriver's job is evaluating payer mix, the amount of practice revenue tied to each insurer. Each month he reviews a report generated by his practice management system showing the percentage of charges for each payer and related collections.
"You need to know how much of a share each payer has of your business, and use that to your advantage from a negotiation standpoint and from an overall contract management standpoint," Schriver says.
Reed Tinsley, an accountant and business adviser to practices, says payer mix evaluations are vital to identifying two key issues: vulnerabilities and opportunities. Evaluating your payer mix identifies potential problems for your practice - suppose there is a major change in reimbursement from one of your larger payers? You can also identify payers who may not be worth working with at all, and those too big to dump but whose low rates cry out for renegotiation.
With data in hand, Tinsley advises practices to be proactive and start improving relationships with those managed care plans. Many practices believe that such discussions will be fruitless, but "you have to try," he advises. Even if you can't negotiate better rates on the first try, he adds, "at least you will come out of those discussions knowing what it will take to improve your reimbursements down the road. You go back to your office, strategize on what it will take to improve and start making those improvements."
You can also walk away from a payer, but should do a full evaluation of the impact of that decision before leaving - or even threatening to leave - a relationship.
When it comes to payment negotiations with payers, there are some key tactics to employ.
Use your leverage. Taylor Moorehead with Zotec Partners, a company providing medical billing solutions, says a successful negotiation is all about leverage. Hospitals use leverage all the time by threatening to decline a payer’s contract outright - forcing patients to pay out-of-network rates or go elsewhere. When patients balk at this prospect, they can become the hospital’s best negotiating ally.
Would such a tactic work for a practice like yours? Maybe, if your practice is large enough, and your payer-mix review reveals a large volume of patients coming from a single, low-paying insurer. But you need to be prepared to actually walk away from a payer before you threaten to do so, and for that you must first understand the consequences of losing a high-volume payer. Run the numbers.
In most cases, says Moorehead, it’s better to seek leverage in other ways.
Promote your uniqueness. Sometimes leverage can come from letting payers know what makes your practice different. The services you offer that no one else in the area does show that you are a unique and valued commodity. Make sure your payers know about them - payers don’t want to lose providers who perform rare services.
Moorehead knows a radiologist who is the only one in a 50-mile radius performing neuroradiology. That’s leverage. But you don’t need to be a subspecialist to be different. The Women's Healthcare Group brought in a registered dietician to give free classes to pregnant patients, something very few OB/GYN practices have in-house.
"This is something we've done to set us apart," Schriver says. "Every practice should have something like that … that increases their attractiveness to a payer."
Data to the payer, about the payer. By conducting a review of your payer mix, not only do you get to know about each payer, but you can also compare your partners across the board. Tinsley says he always brings data on the payer to negotiations and, sometimes, will ask for data from the payer.
Schriver says the "best tool at my disposal" is a spreadsheet he has created showing all the fees for all of the codes his practice bills, listed by payer. "There is no better way, in my mind, to truly evaluate, in relative terms, what we are getting paid."
"You really need to know where they rank in relation to all of the other payers, code-by-code, looking for an aggregate percentage of Medicare," Schriver adds. "You definitely have to go into any discussion with that data."
Our Fee Schedule Survey data, presented throughout these pages and in greater detail at PhysiciansPractice.com, adds a second dimension to such an analysis: Your own data clarifies how well each of your payers pays you in relation to other payers. Our data helps you understand how well each pays you compared with other practices in your market.
But knowing how much you're paid is only part of the equation when assessing payers' value. You should also examine how easy they are to work with, how often they deny claims, how long they take to pay you, and other important "hassle factors," all tracked and ready when you need them. Physicians Practice offers data on this, too, each year with its Payer View report.
Schriver adds that given the current reimbursement climate, "it becomes more and more clear to me that I have to come to the table with lots of tools to discuss fee schedules with that payer."
Have the right attitude. Often times, asking anyone for money can be tough, but it doesn't have to be confrontational. Tinsley tells his clients to understand that payers don't want to give money away, so the best attitude to take is, "if you scratch my back, I'll scratch yours."
In other words, let the payer know why you deserve more money and the positive result of a better relationship. He cites a group with four urgent care centers. By using data, he was able to show that these offices were keeping patients out of the local ER and that avoiding those visits benefited the payer, who would pay more to the hospital, so the centers got a better reimbursement rate instead.
"My attitude is, 'I'm going to ask you for this money, but in return, how can I work with you to improve the delivery of healthcare on my end to reduce costs because you too are going to save money on your end?'" Tinsley says.
Moorehead adds that if you are looking for an ally in negotiations, appeal to the one person at the insurer who knows the position you are in: the physician medical director. While this person may have no role in setting rates, he may be able to vouch for the way you code for a procedure or the unique services you provide for the network.
"Go physician-to-physician," Moorehead says. "I’ve gotten groups to meet with medical directors to negotiate rates and almost every time, it has worked."
Government relations
Of course, you can't really negotiate with the government the way you can with payers. Medicare and Medicaid are take-it-or-leave-it when it comes to rates.
What you can do, however, is use the same evaluation tactics to determine whether the time has come to decline to see any new Medicare patients, or to end your relationship with Uncle Sam entirely. If you do stick with the government payers, you can at least be sure that you’re getting paid what you're owed.
"If you are supposed to get $500 and you are getting $495, you’re being shorted $5 every single time and if you are looking at thousands [of claims], you better be checking," Moorehead said.
Robert Hill, Jr., a principal with Philadelphia-based Health Strategies and Solutions, agrees with Moorehead that checking payments and all transactions at the end of the month is a good idea to be sure you are getting all you were promised from the government.
If you are not getting paid what you agreed upon, you have the right to appeal. Yet Schriver also notes that practices have to stay on top of payer policies, making sure a staff member keeps up with e-mail bulletins and newsletters informing them of changes in policies and the impact on coding or reimbursement.
"The most important thing, as a starting point to making money" is CPT coding, says Tinsley. "It is amazing how poor physician offices are by not billing everything they are entitled to get paid for. CPT coding is everything."
Access incentives
Hill also advocates working to optimize any payer incentives which can include data tracking, shifting to later hours of operation, accepting sick clinic and walk-in patients, and EHR integration.
"All that can help you optimize payments from various payers," Hill says.
Since 2007, Idaho Emergency Physicians in Boise has participated in Medicare's Physician Quality Reporting Initiative (PQRI) - which provides incentive payments in return for data on quality measures for services to Medicare beneficiaries.
Lisa M. Jolliff, the practices' coding manager and compliance officer, says her staff of certified coders reads the charts, abstracts, and reporting items as necessary, and in addition to CPT and ICD-9 codes, adds the PQRI codes to report this data to the federal government.
She concedes it took some money to adjust the practice's practice management software, as well as the cost of training for staff to get used to taking a few more steps with each patient record. But the result of those few more steps - which are now second nature to the coders - has resulted in $20,000 from the PQRI program in 2009.{C}
"That's $20,000 more than we had," she says, "so why would we leave those dollars on the table? Why leave it there if it is available to you?"
But with possible cash comes caution, as Jolliff says, practices need to see if participating in PQRI and other pay-for-performance programs are cost-worthy, balancing the cost to implement additional reporting with what they could get in return. If participation means thousands of dollars on technology upgrades or even a new system, or, hours of staff training or hiring additional staff, it may not be worth it.
And then there are looming federal incentives for adoption of certified EHRs, with practices anticipating certification of their systems or word that they need to buy new ones in order to meet the government's "meaningful use" guidelines.
Hill says that meaningful use of EHRs can have the double benefit of bringing in federal incentive dollars while also helping practices audit payments and compliance with their various payers.
Baby steps
Working with payers for greater reimbursement, making sure the government is paying you everything you are owed, and taking advantage of incentives from public and private payers are all key elements in maximizing your revenue appropriately for the work you do.
"People need to focus on the different pieces of the revenue cycle," advises Louis D. Papoff, chief financial officer of physician services for Vanguard Health Systems, which owns hospitals and physician groups in the Chicago area. "They are all important and perhaps the best way to break things down is to do so in the tiniest pieces and make sure each of those pieces is being done correctly."
Editor's note: Staying afloat means collecting every dollar you're owed. For tips on collecting from patients, read "Getting Patients to Pay."
In Summary
To get paid more for the work you do:
• Monitor your payer mix. Knowing who your larger payers are ahead of time can help you assess the impact of rate cuts.
• Show payers what sets your practice apart, from ancillary services to add-ons.
• Take advantage of federal incentive programs.
• Train staff to discreetly discuss patient balances and past due balances at the time of service.
Keith L. Martin is associate editor at Physicians Practice. He can be reached at keith.martin@ubm.com.
This article originally appeared in the January 2011 issue of Physicians Practice.