Understanding Health Insurance Payer Performance
The latest data from PayerView, the annual ranking of insurers from billing services and software company athenahealth, shows payer performance in decline. But what about your payers? Here's advice on how to monitor the performance of your own top payers, plus key data from national and regional payers.
Is your practice struggling to monitor payer performance? You may share Barbara Sack's view.
"Some days [monitoring payer performance] seems like the bane of my existence," says Sack, administrator of Midwest Orthopedics in Shawnee Mission, Kan. "It's another reason that it now takes more billing people than clinical people to see a patient, which is a frustration for all of us in healthcare."
When approaching the task of monitoring payers more closely, consider the advice of P. J. Cloud-Moulds, owner of Medical A/R Recovery, and a blogger on PhysiciansPractice.com.
"Just like a doctor might say to a patient, 'this is going to hurt but, in the long run, you are going to feel better,'" Cloud-Moulds says.
Some practices focus too much on payment rates when considering the value of their payer contracts, giving too little consideration to payer performance as defined by payment timeliness and accuracy, administrative hassles, denial rates and reasons, and more. Understanding a payer's performance as a partner in your business requires a complex and nuanced analysis of metrics that haven't always been easy to come by.
Yet for most practices, monitoring payer performance is usually worth the time and effort, even if it requires more staff, experts say.
You can simplify matters by focusing only on your biggest payers: Create a basic spreadsheet with your most important private payers and, within that set, scrutinize only those payments for the services that make up the majority, say 85 percent, of your practice's gross charges. It may be as few as 25 or 30 CPT codes.
Although even that number of codes can be onerous to monitor on a regular, payer-by-payer basis, consider the potential payoff of a careful performance-monitoring program: major commercial health insurers had an average claims-processing error rate of 19.3 percent in 2011, up 2 percent from the previous year, according to an analysis by the AMA.
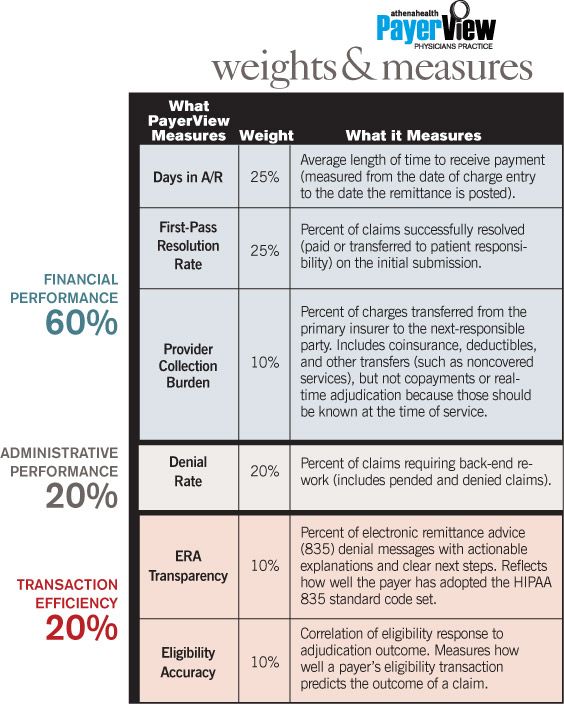
And in athenahealth's just-released PayerView report, an analysis of payer performance based on real claims data from the national billing and practice management services company, payer performance has been declining as insurers shift resources away from improving their claims-management process and toward meeting new government regulations. Joe Hendrickson, vice president of athenaNet Intelligence, which compiles the annual PayerView data, says that the company's analysts are not expecting payer performance to improve next year. In fact, after several years of steady improvement following the debut of PayerView in 2005, it's possible that payer performance has more or less topped out, Hendrickson suggested.
The latest edition of PayerView, found that payers, overall, are taking longer to pay, that fewer claims are getting paid on their first submission, and that higher percentages of what's owed to practices are being pushed onto secondary insurers and other parties from which the practice must seek payment separately.
In other words, athenahealth found, it's getting harder to get paid.
*How are your payers performing? Find out with our in-depth national and regional data: Blues / Major Payers / Medicaid / Medicare / National Commercial / Midwest / Northeast / South / West. This information is also available at athenahealth.com.
Four-point plan
Cloud-Moulds suggests that any program for assessing payer performance should include tracking the number of days each of the major payers' claims spend in accounts receivable (A/R). Faster pay means better cash flow. Additional areas can include watching for:
• Inappropriate application of coding edits;
• Overlooked modifiers; and
• Unjustifiable bundling of services.
Billing services and software programs can help with many of these tasks, but you may still need additional staff to manage the effort and make it pay off, Cloud-Moulds says.
"It's more monitoring and I'm sure that when we talk about it, the doctors are thinking, 'My staff is already too busy to do all of this monitoring,'" Cloud-Moulds says. "Adding a new position is certainly going to hurt a bit upfront but it will save you so much more in the long run."
It's tempting to jump right into the payer-monitoring effort by devising a report card, but make sure to get a few things in order first, says Dan Rodriguez, founder and president of Kareo, a practice management and medical billing software firm.
Rodriguez suggests a four-point plan to lay the groundwork for spotting payer payment inaccuracies.
1. Get familiar with contracted rates. "Trust but verify," Rodriguez says. "We still see a lot of practices taking it on faith that they are going to get paid accurately instead of approaching this relationship with a healthy skepticism."
Because each payer has its own take on payment rules, coding, code modifiers, bundling, and so on, it's important to know what your contracts say. Keep a basic spreadsheet that shows contract highlights, he says. (See the box "The Contract Spreadsheet.")
2. Use accurate fee schedules. Obtain data files of the fee schedules from your largest payers. Focus on your most common 20 to 30 procedures, or those that make up the majority of your gross revenue, Rodriguez says. Load those payer schedules into your practice management system or, at the very least, keep a basic spreadsheet for the top four or five payers by volume. If you are contracted to receive a percentage of Medicare, make sure the payer uses the proper year's Medicare physician fee schedule and does the math correctly, Rodriguez says.
3. Reconcile. If you can use an automated payment reconciliation system tied into your practice management system, it may not be hard to crank out daily reports showing variances between expected and actual payments. A billing service also may offer this feature.
Restricting oversight to just your largest payers and your most frequently billed codes will make good sense if you must monitor via the spreadsheet route instead of a fully automated solution. A more limited view also makes sense if your electronic data systems are not well integrated and require hands-on attention to produce variance reports. In those cases, conducting sampling audits of your five largest payers by volume will be worth the effort, Rodriguez says.
"Auditing for these variances can uncover some very attractive revenue," he says. "Our customers who are doing these things are collecting 12 percent more on average in insurance billing."
4. Take action. When it comes to filing appeals, many practices simply run out of time to handle the workload before an appeals deadline closes. Often, they lack sufficient staff to push all the paperwork and have not tried to automate the process. Even creating a small repository of template appeal letters will help (download the sample appeal letters at Physicians Practice Tools).
Key indicators
While you are hard at work looking for mismatches between contracted rates and actual reimbursements, there are other components of the payer-medical practice relationship to watch. They include:
• Aging A/R. Track by payer and watch for those whose days in A/R (time between claim submission and payment) are increasing or remain stuck at levels above industry averages.
• Denials. At least once a month, pull reports from your practice management system to show all denied claims. Sort by payer, denial reason, and dollar amount. Patterns may emerge to show if it is the practice or the payer causing the problem. Be wary of medical necessity denials and studiously appeal each inappropriate denial.
• Write-offs. By monitoring EOBs, you are more likely to avoid writing off a portion of a charge when you should have appealed. Your staff may be writing off a health insurer's unfounded discounts instead of reworking those claims or filing appeals. A payer may cause noncovered service-related write-offs to increase by separating certain items (such as an EKG) from its coverage of routine preventive exams.
Subjectivity counts
While the focus is often on the hard facts of payer performance, a report card is more useful with qualitative input.
Lucien Roberts, vice president of Pulse Systems, Inc., and a former practice administrator, suggests asking each employee in the practice to grade the major payers from A to F. Graders should include everyone who touches anything to do with a payer - front desk check-in, billing office, physicians, nurses, medical assistants, referral nurse, and so on.
"Ask them to assign the grades based on what it's like dealing with that payer from their unique perspective," Roberts says. Also ask graders to write comments on why they've given a high or low grade.
The goal of the subjective report card, Roberts says, is to give the practice's administrator a much better feel for what it is like to work with that payer. With these insights in hand, the administrator is in a better position to advise the practice's leaders when the time comes for the practice to decide whether to renew a contract, try to renegotiate it, or let it drop.
The contract spreadsheet
You can build a sophisticated database or buy specialty software, but many medical practices find that a basic Excel spreadsheet program meets their needs for keeping track of payer contracts.
The spreadsheet should list the:
• Payer;
• Product type (PPO, HMO, etc.);
• Effective dates;
• Rates and conditions, such as percentage of Medicare for E&M codes and carve-out for other services;
• Amount of inflation adjustment factor (if any); and
• "Gold card" status services, if any (often for specialists - specific services or codes where preauthorization is not required).
*How are your payers performing? Find out with our in-depth national and regional data: Blues / Major Payers / Medicaid / Medicare / National Commercial / Midwest / Northeast / South / West. This information is also available at athenahealth.com.
Robert Redling is a freelance writer based in Tacoma, Wash. He has been practice management editor for Physicians Practice, Web content editor and senior writer for the Medical Group Management Association, and a speechwriter for the American Academy of Family Physicians. He can be reached via editor@physicianspractice.com.
This article originally appeared in the July/August 2012 issue of Physicians Practice.