Thoughts on CMS’s dramatic proposal for E/M guidelines
Here are five reasons why CMS’s proposed Physician Fee Schedule for Evaluation and Management guidelines might improve patient care.
CMS has released proposed changes to the Evaluation and Management (E/M) coding guidelines. I have long been a critic of the complexity and subjectivity of the current guidelines. However, I think these changes will be both a good thing and a challenge to physicians, particularly those who derive much of their income from office visits.
CMS has proposed to bundle both established patient visit codes 99212 through 99215 into a single code and new patient visit codes 99202 through 99205 into a single code. The lowest established and new patient visit codes, 99211 and 99201, would remain, but given the small frequency with which they are used, the biggest impact to physicians will be from provided care under the bundled codes.
The following chart shows Medicare’s national average current and proposed payments:
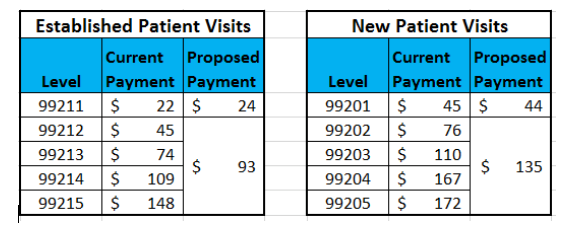
The proposed payment for each type of service is between the current level 3 and level 4 payments. An additional $5 add-on payment per visit has been proposed for primary care services-both established and new-though details are lacking at this point.
Here are my five impressions of the proposed rule that, if passed, would take effect Jan. 1, 2019. A summary of the proposed changes is available from CMS, and the full proposal is availble on the Federal Register.
The winners and losers
There is a lot of money at stake. Though CMS’s proposed changes are budget neutral, there will be winners and losers in this zero-sum game. Physicians who frequently code level 4 and 5 services will see a decrease in E/M reimbursement, as the proposal sets future service payment at less than the current reimbursement rate for level 4 services. Conversely, physicians who code the majority of their services as level 3 will see their E/M reimbursement go up since the services will be paid at more than the current reimbursement for level 3 services.
Objectivity at last
It has been more than 20 years since the 1995 and 1997 E/M guidelines were promulgated. Studies by Mitchell King, MD, and others have shown that coding E/M services is subjective and confusing. Fewer than 6 in 10 physicians would code an office visit at the same level though, oddly enough, King’s research found only a slightly better average for certified professional coders. And yet, Medicare and other payers have penalized physicians for overcoding using Recovery Audit Contractors, chart audits, and other tools. Those days of selecting the wrong code and thus being accused of fraud should go away under the proposed plan. That is a very good thing.
No more note bloat
The new codes will require minimum documentation, enough to meet what is needed today for a level 2 visit, and that’s it. Physicians can focus on what has changed rather than redocumenting what has not. All of the note bloat that adds nothing to patient care-and is glossed over by anyone receiving your note, anyway-will be marginalized. You will be able to review and verify information you, your staff, or your patients entered rather than redocumenting it. I won’t go so far as to suggest you’ll enjoy documenting, but I think you’ll find it much better when your notes are more concise and meaningful.
Budget neutrality beats the alternative
Since the advent of click-and-count documentation in EHRs, the use of level 4 and 5 codes has nearly doubled. They account for almost half of all E/M services today and have been trending steadily upwards for nearly 20 years. Maintaining budget neutrality within the E/M realm was not a given, and I am happy that some E/M monies were not reallocated to non-E/M services.
Care will improve
We, the community of providers, can now focus on our patients and on documenting what really matters: the care provided and the care plan. Documentation will be better and, I think, easier. Notes received from other doctors will be similarly streamlined and-dare I say-cogent. I really believe both patient care and coordination of care will improve.
Like the Lorax, I have spent years advocating for changes that seemed obvious to me but oblivious to those in power. CMS is at long last moving in the right direction. There will be losers, this being a zero-sum game, but these proposed changes are good for all of us and our patients. I believe that, and overall, I am pleased with CMS’s proposal.
Lucien W. Roberts, III, MHA, FACMPE, is administrator of Gastrointestinal Specialists, Inc., a 25-provider practice in Central Virginia. He may be reached at lroberts@gastrova.com.
The benefits of direct primary care
March 25th 2025Direct primary care is transforming the healthcare landscape by replacing insurance-driven models with affordable, membership-based care that strengthens patient-doctor relationships, reduces costs, and improves access to personalized treatment.


