National Healthcare Decisions Day reminds us why “Having the Conversation” is critical
Honest conversations about end-of-life care.

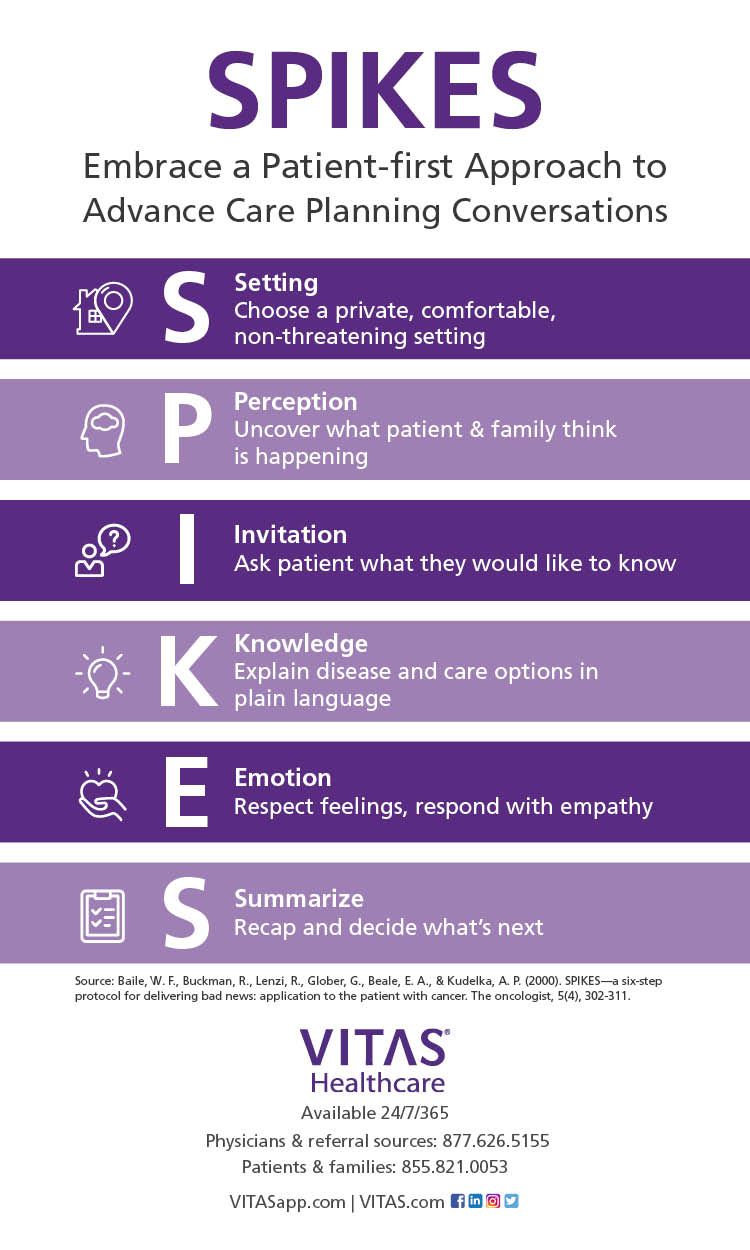
SPIKES Patient Conversation Technique; Click to View
As the nation prepares for National Healthcare Decision Day on April 16, the COVID-19 pandemic reinforces the value of honest conversations among physicians, their patients, and family members about wishes, goals and values for end-of-life.
Almost daily, heartbreaking news stories describe patients who are dying alone, in a nursing home, hospital, or intensive care unit, without their family members able to visit or stand vigil. Just as this pandemic underscores the stress on the nation’s healthcare workers and infrastructure, it also serves as a stark reminder of the consequences of physician discomfort and unease about “having the conversation” with patients about the care they want-and do not want-if they face a serious disease or are unable to communicate near the end of life.
Ask most physicians why they have chosen a career in medicine, and they’ll say they want to help people. COVID-19 reminds us that part of helping people is honoring their wishes and that not talking about their goals and not following their wishes is not helpful, especially near the end of life.
Trending: How have a well-run practice
At VITAS Healthcare, we believe speaking honestly with patients is essential, especially when the conversation involves difficult news or equally difficult decisions about end-of-life care. Goals-of-care conversations and advance care planning are proven activities that support patient-centered care.
Studies as recently as 2018 (El-Jawahri et al, Circulation) and 2016 (Patel et al, JAMA Oncology) have shown that advance care planning results in increased hospice utilization, fewer hospitalizations near the end of life, fewer visits to the emergency department and ICU, all without increasing psychological distress such as depression and anxiety in patients. Likewise, patients who engage in end-of-life conversations also have a better understanding of their illness and are more willing to complete living wills and healthcare power-of-attorney designations.
The VITAS commitment to transparency means that we remind our physician colleagues to rely on hospice and palliative care specialists, and tools like the SPIKES (Setting, Perception, Invitation, Knowledge, Emotion, and Summary) Protocol, to initiate and complete goals-of-care conversations with patients and families. SPIKES was developed by the University of Texas MD Anderson Cancer Center in Houston, Texas. Pioneered by Robert A. Buckman, M.D Ph.D., the six-step format provides clear direction for honest, rewarding conversations about care preferences between doctors and their patients and families.
It helps to think of SPIKES and similar tools as frameworks for starting, continuing, and completing goals-of-care conversations. These tools help physicians improve their communication skills and feel increasingly comfortable engaging in them. The resulting care plan defines what end-of-life care will look like and who is responsible for making decisions.
SPIKES: A step-by-step guide to "having the conversation"
The SPIKES acronym calls for the proper setting (S), perception of the patient/family understanding of the disease (P), an invitation (I) by the patient to receive more information, knowledge (K) from the physician about care options, emotional (E) and empathetic responses by physicians, and a summary (S) care plan to move forward. SPIKES achieves key goals:
- Assess the patients’ level of understanding of their disease, and their willingness to receive news
- Ensure the information being shared is easy to comprehend.
- Minimize the emotional impact of the news by reacting with empathy
- Develop a care plan that the patient understands and supports
SPIKES empowers physicians and clinicians to have thoughtful conversations with patients about care options and end-of-life care. The very nature of the medical profession, however, means it’s often hard for physicians to let go of the “cure” piece and replace it with the “care” piece. Hospice and palliative care professionals specialize in the “care” piece.
Having a goals-of-care conversation is not about giving up or feeling like a failure. It is an act that honors patients and respects them for who they are. It is a powerful tool that helps patients by embracing their values, goals and preferences. It is an activity that can bring us back to our core mission to help our patients.
Read More: Five Medicare Services to Keep Your Patients and Practice Healthy During COVID-19
Ideally, physicians who engage in these conversations will know what their patients want in the face of a serious illness and can refer them to hospice care. Patients with COVID-19 or any other advanced illness can be cared for at home, allowing them to be in the place they prefer to be, with the people they prefer to be with, and able to experience quality of life near the end of life.
No physician should ever feel uncomfortable “having the conversation” about end-of-life care with patients and their families. Helpful tools like SPIKES can support and deepen the necessary skills, and hospice specialists are available 24/7 to have the conversation for those who do not feel comfortable or capable of doing it well.
Talking about end-of-life care is, in fact, one of the most helpful things physicians can do.
Joseph Shega, MD, is senior vice president and chief medical officer for VITAS Healthcare, the nation’s leading provider of end-of-life care. Dr. Shega is responsible for oversight of the regional medical directors, the director of physician services and overall medical direction at VITAS programs in 14 states and the District of Columbia.
Reducing burnout with medical scribes
November 29th 2021Physicians Practice® spoke with Fernando Mendoza, MD, FAAP, FACEP, the founder and CEO of Scrivas, LLC, about the rising rates of reported burnout among physicians and how medical scribes might be able to alleviate some pressures from physicians.